ABSTRACT
OBJECTIVES: to analyze the spatial distribution for stillbirth and spatial association with women's health and social vulnerability indicators in the city of São Paulo, Brazil.
METHODS: ecological study of administrative districts of the city of Sao Paulo, from 2014 to 2021. The outcome is the stillbirth rate, and covariates are mother's age, inadequate prenatal care, the Paulistan Social Vulnerability Index (PSVI), women in childbearing age, mortality rate and birth rate. Exploratory spatial analyses included crude and Bayesian stillbirth rates. Spatial autocorrelation was tested using t Moran's index and Geary's coefficients. Local Indicator of Spatial Association and Moran scatterplot were used to identify the risk areas. The Lee coefficient was used to correlate the indicators with stillbirth.
RESULTS: a total of 39 low-risk clusters were identified in the central region, while 40 high-risk clusters were identified, primarily in the eastern region (p<0.05). Higher social vulnerability, higher proportions of adolescent mothers, and higher mortality rates among women of childbearing age were significantly correlated with higher stillbirth rates (p<0.05).
CONCLUSIONS: the analysis identified the areas where higher social vulnerability, higher proportions of adolescent mothers and higher mortality rates of women of reproductive age are correlated with higher stillbirth rates.
Keywords:
Spatial analysis, Fetal mortality, Social vulnerability, Correlation of data
RESUMO
OBJETIVOS: analisar a distribuição espacial da mortalidade fetal e sua correlação com indicadores de saúde da mulher e de vulnerabilidade social na cidade de São Paulo, Brasil.
MÉTODOS: estudo ecológico dos distritos administrativos no período 2014-2021. Desfecho: taxa de óbito fetal; covariáveis: idade materna, cuidado pré-natal inadequado, Índice Paulista de Vulnerabilidade Social, taxas de óbito em mulheres em idade reprodutiva e de natalidade. Análises espaciais exploratórias incluíram taxas de mortalidade fetal brutas e Bayesianas. A autocorrelação espacial foi testada pelo índice de Moran e coeficientes de Geary e a identificação de áreas de risco pelo Índice de Moran Local e pelo diagrama de espalhamento de Moran. Correlações entre indicadores e mortalidade fetal foram obtidas pelo coeficiente de Lee
RESULTADOS: foram identificados 39 distritos de baixo risco na região central como clusters de baixo-baixo risco e 40 distritos como clusters de alto-alto risco, principalmente na região leste (p<0.05). Identificou-se que maior vulnerabilidade social, mães adolescentes e a mortalidade das mulheres em idade fértil estão correlacionadas com maiores taxas de mortalidade fetal (p<0.05).
CONCLUSÃO: a análise identificou as áreas em que a maior vulnerabilidade social, maiores proporções de mães adolescentes e maiores taxas de mortalidade em mulheres em idade fértil estão correlacionadas com taxas mais elevadas de mortalidade fetal.
Palavras-chave:
Análise espacial, Óbito fetal, Vulnerabilidade social, Correlação de dados
IntroductionAccording to Chou
et al.,
1 the global stillbirth rate in 2019 was 13.9 per 1000 births, down from 21.4 per 1000 born in 2000, indicating a decrease of 35.1% over nearly two decades. Recent data show around 1.9 million fetal deaths worldwide in 2023,
2 down from 2.6 million in 2015,
3 continuing this downward trend.
The literature reveals the importance of measures concerning stillbirth prevention and reduction. However, this subject has been neglected
4 and was included in the global health agenda only in 2014, with Every Newborn Action Plan (ENAP), which aims to eradicate preventable maternal, fetal, and neonatal deaths by 2030. In the state of São Paulo (SP), significant disparities exist, with 42% of cities reporting higher stillbirth rates than neonatal mortality. Projections suggest that stillbirths may surpass neonatal mortality across Brazil in the medium to long term, driven by recent improvements in neonatal care and the increasing focus on stillbirth prevention.
5Regional contrasts for fetal and neonatal mortality rates in Brazil are associated with coverage, utilization, and access indicators of the national Unified Health System services (SUS – Portuguese acronym), pointing to a higher frequency of system failures of childbirth and puerperium care in the North and Northeastern regions of the country.
6 These results highlight the importance of the use of spatial-temporal monitoring in identifying patterns for better organization of maternal and child programs.
Measures of spatial correlation to identify these associations have been employed in identification of patterns. Canutto
et al.
7 showed the increasing gradient of the index of social deprivation with the increase of the stillbirth rate, ranging from 8.0-10.7 per 1000, in the mesoregions of São Francisco and Sertão, in the state of Pernambuco. Marques
et al.
8 found an association of avoidable causes of fetal deaths and three clusters of social vulnerability obtained from the Paulistan Social Vulnerability Index (PSVI) distribution in the districts of the city of Sao Paulo, from 2007-2017. Venâncio
et al.
9 identified perinatal mortality patterns in the state of SP by the Moran’s index, identifying municipalities with the highest risk. Nascimento
et al.
10 evaluated the spatial dependency for the perinatal mortality in areas with lack of pregnancy care, in 63 areas in the city of Salvador, by Global and Local Moran’s index and Geary’s coefficient, in 2007. Silva
et al.
11 identified that fetal mortality in the city of Recife was correlated to the Social Vulnerability Index (SVI) that considered three factors: “income and work”, “urban infrastructure” and “human capital”. Silva
et al.
12 evidenced a spatial correlation between fetal mortality rates and health districts, highlighting regional disparities and the need to identify these areas for targeted health policies.
The city of São Paulo, a metropolis of 12.2 million inhabitants, with large socioeconomic disparities between the 96 administrative districts (AD) and concentrates 28.9% of the stillbirths of the state of SP from 2014
-2021. In the state of SP, the stillbirth rates are an increasingly important component of perinatal mortality with the continuing decrease in early neonatal mortality.
5In this paper, we present the analysis focusing on using the indicators obtained from the districts, without aggregating them in clusters that would comprise large areas and population, which would cause a higher heterogeneity. Most of the papers found approached spatial correlation in larger areas, especially to stillbirth.
This study aims to identify high-risk areas for fetal mortality and use regional indicators as key tools for public policy planning, enabling targeted actions to reduce preventable fetal deaths.
MethodsThe study design is an ecological and exploratory study that assessed live births and stillbirths from mothers residing in the city of São Paulo from 01/01/2014 to 12/31/2021. The administrative districts of the city were defined as the unit of analysis in the present study. In the analysis, the residents from 2014 to 2021 were considered and data without any information were excluded.
The outcome variable is the stillbirth rate for each district, it was obtained from the Mortality Information Improvement Program (PRO-AIM – Portuguese acronym) of the Coordination of Epidemiology, and Information (CEInfo) of the Municipal Health Department of São Paulo through the TabNet.
13 The stillbirth rate is the number of stillbirths per 1000 live births.
The exposure variables considered the following indicators:
a) Percentage of inhabitants in medium, high, or very high social vulnerability conditions: The PSVI is an index to measure social vulnerability and classifies the districts of the city into 6 clusters that range from very low to very high vulnerability, carried out by the State Data Analysis System Foundation (SEADE – Portuguese acronym),14 in 2010. The index reflects economic and social performance data, comprising income, education, access to public services, opportunities for social mobility and admission conditions in the job market. The PSVI is an ordinal qualitative variable comprising seven social vulnerability groups: extreme low, very low, low, medium, high (urban), very high and high (rural), using available information on the frequency distribution of the inhabitants of each district in the defined groups. A function was constructed from the sum of the relative frequencies for the medium, high, and very high groups.
b) Percentage of adolescent mothers: ratio of the number of women aged 19 years or less who have had at least one live birth per the total number of women who had children. Source: Live Birth Information System (SINASC – Portuguese acronym),13 from the Ministry of Health of Brazil.
c) Percentage of mothers with inadequate prenatal care: ratio of the number of mothers who did not undergo prenatal care or who went to less than seven prenatal consultations per total number of women who have had children. Source: SINASC.
d) Mortality rate of women in childbearing age: ratio of the number of deaths of women aged 15-49 per total number of women in the age group. Source: PRO-AIM. Data available from 2014 to 2019.
e) Birth rate: ratio of the number of live births per total population, multiplied by 1000. Source: SINASC.
All variables were calculated using the average between 2014 and 2021, while the PSVI was constructed using variables related to 2010.
The digital SP network per district was obtained at the Geosampa online platform, available free of charge by the São Paulo Municipal Government in shapefile format (shp).
15The exposure variables considered indicators relied on other perinatal studies, such as education and mother’s age, a socioeconomic variable as PSVI. The birth rate is a proxy for the size of the district and the presence of health services in the district. We also included the mean monthly income as a traditional economic variable.
Statistical methods: the crude and empirical Bayesian stillbirth rates were calculated for the districts, followed by construction of thematic maps for each rate. Global Empirical Bayesian stillbirth rates aim to minimize random fluctuations in crude mortality rates observed in the analysis units. The Local Empirical Bayesian Estimator considers the rate adjustment of each district by the rates of its neighbors, applying a neighborhood matrix. The empirical Bayesian method considering information of the neighborhood and relations between close areas in small populations, by allowing a better control of the variability of rates through the reduction in variance.
16 A Queen type neighborhood matrix was used for the spatial analysis, which considers adjacent districts with at least one common border point as neighboring, regardless of the direction of the points.
16The Global Moran’s index and Geary’s coefficient were calculated to verify evidence of spatial autocorrelation concerning fetal deaths in SP: the first uses the difference between each point and the global average, while the second uses the difference between pairs of points. The Global Moran’s index ranges from -1 to 1 and has similar interpretation as the Pearson correlation. Global Geary’s coefficient ranges from 0 to +2, with values between 0 and +1 indicating positive spatial autocorrelation and values between 1 and +2 indicating negative spatial autocorrelation.
17The Local Indicator of Spatial Association (LISA)
17 deconstructs the global indices, detects non-stationary regions and groups neighboring areas with similar indices to find significant clusters. The local Moran Index identifies risk areas for stillbirth. A thematic map of the standardized index (z-score LISA), by district, and a thematic map highlighting the districts with their respective significant indices are presented.
The Moran scatter plot
16,17 allows for the identification of four types of spatial linear association of coverage areas: high-high (HH), high-low (HL), low-low (LL), and low-high (LH). This graph is obtained by the distribution of the crude stillbirth rates by the respective spatial first-order lag rates. LL clusters identify low-value stillbirth rate districts surrounded by low-value stillbirth rates, as well as the opposite, districts with high rates surrounded by high rates represent HH municipalities. The transitional clusters LH and HL stand for low-rate districts with neighboring higher value areas and higher rates but with low-rate neighbors, respectively.
Finally, the correlations between each secondary indicator and the crude stillbirth rates were calculated by the Lee coefficient, as bivariate spatial association,
17 combining the Moran’s index and Pearson’s correlation definitions. The Lee coefficient ranges from -1 to +1, with interpretation equivalent to the Pearson’s coefficient.
The thematic maps and data analyses were processed in the software R 4.2.2.
The research protocol was approved by the Research Ethics Committee of the University of São Paulo, belonging to the Public Health School, CAAE 87655518.6.0000.5421, approval number 2.667.915, on May 22, 2018.
ResultsFrom 2014 to 2021, 10,263 stillborns and 1,294,412 live births were registered in SP, with a crude stillbirth rate of 8.24/1000 births.
The percentage of missing data due to the absence of the administrative district was 0.16%. For those with information about the district there were no missing values. No fluctuations or trends over time of the stillbirth rate were observed, with the lowest rate observed in 2018 (7.54/1000 births) and the highest, in 2021 (8.40/1,000 births), with mean of 7.88 and standard deviation of 0.27. Considering this small variation and the fact that stillbirth is a rare event, we considered the sum of the data from 2014 to 2021 (Figure 1A). The crude rate variance was reduced, reflecting the reduction of random fluctuations concerning risk for stillbirth in the districts (Figure 1B). Local empirical Bayesian stillbirth rates, which are also smoothed, and the neighborhood-weighted rates are displayed in Figure 1C.
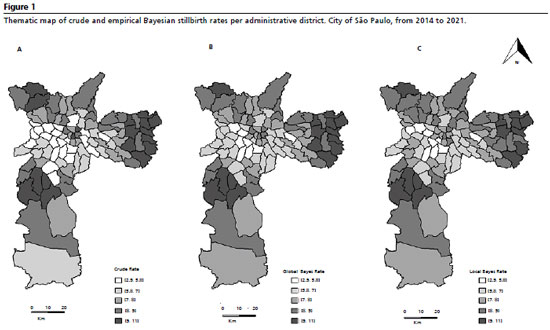
The crude, the global and the local Bayesian rates follow similar geographic distribution (Figure 1), where the stillbirth rates increase towards the more peripheral districts, forming high-risk clusters in the Eastern and Southern regions, and low risk clusters in the central region. According to the global Bayesian rates (Figure 1B), the districts with the highest rates of fetal death, between 9.27 and 10.2/1000 births, are Cidade Tiradentes, Vila Jacuí, Iguatemi, Itaquera, Itaim Paulista, Lajeado and Jardim Helena, located in the eastern zone and Socorro, located in the south zone of the municipality. In contrast, the lowest rates of global empirical Bayesian stillbirth - between 4.8 and 5.7/1000 births, were observed at Pinheiros, Jardim Paulista, Perdizes, Itaim Bibi and Lapa, in the western zone; and Carrão, Vila Mariana and Moema, in southeastern.
The Global Moran’s index and Global Geary’s coefficient were calculated using crude rates, with estimates of 0.5822 (
p<0.05) and 0.4346 (
p<0.05), respectively, which evidence of spatial autocorrelation among districts in relation to the stillbirth rate. The standardized Local Moran’s index (Figure 2A) identified the district clusters with significant spatial dependence and ranged between -1.55 and +4.45, corresponds to
p-values between 0.96 and <0.0001, and a value of 1.99 relates to a
p-value of 0.05. Figure 2B displays a cluster in the Eastern region and another in the Western region, with significant rates (
p<0.05), comprising 28 districts, 12 with a high prevalence of stillbirth rate – so that 11 in Eastern region, and 16 characterized by low stillbirth rates – so that 12 in Western region.
The high-risk cluster identified by the LISA index comprises the following districts: Cidade Tiradentes, Guaianases, Iguatemi, Itaim Paulista, Itaquera, José Bonifácio, Lajeado, Parque do Carmo, Ponte Rasa, São Miguel and Vila Curuçá, located in the Eastern Zone of the municipality, and Cidade Dutra, in the Southeastern Zone. The low-risk cluster comprised Consolação, in the Central Zone, Alto de Pinheiros, Butantã, Itaim Bibi, Jaguara, Jaguaré, Jardim Paulista, Lapa, Morumbi, Perdizes, Pinheiros and Vila Leopoldina, in the Western Zone, Moema, Saúde and Vila Mariana, in the Southeastern Zone, and Campo Belo and Santo Amaro, in the south zone (Figure 2).
The Moran scatterplot (Figure 3A) evidence spatial autocorrelation, presenting spatial associations and concentration patterns. Figure 3B shows all types of clusters, LL and HH clusters. This indicates that low-value stillbirth rate districts are surrounded by low-value stillbirth districts and
vice versa. A total of 40 districts were in HH clusters, located in the peripheral regions at the East, Eastern, North, South regions (Figure 3B). The LL cluster concentrated 39 districts in the Southeast and West regions of the city.
Clusters considered as transition groups were formed by low-rate districts with neighboring areas presenting higher values (LH), totaling six districts, each belonging to a different region of the municipality - North, South and Southeast - and those comprising districts with higher rates but adjacent to low (HL) districts, located in the North, South, Southeast and Center regions, totaling 11 districts.
Figure 4 presents the thematic maps of each of the six district indicators in SP. High distribution values of inhabitants in conditions of medium, high, or very high social vulnerability were noted in the peripheral regions of the municipality. Similar patterns were observed concerning the distribution of percentages of adolescent mothers and mothers with inadequate prenatal care, birth rates, and mortality rates in women of childbearing age. However, an inverse spatial pattern was observed regarding average monthly income, with higher indices in the central regions.
Table 1 presents the Global Moran’s index for each indicator, with estimates ranging from 0.304 to 0.700, all significant (
p<0.05), showing the evidence of spatial autocorrelation between districts in relation to all secondary indices. These results suggest a correlation between stillbirth rates and secondary indicators. Initially, Pearson correlation coefficients were calculated between each indicator and crude stillbirth rates. Table 1 shows that indicators positively and moderately correlated to crude stillbirth rates were “proportion of adolescent mothers”, “proportion of mothers with inadequate prenatal care”, “mortality rates in women of childbearing age” and “proportion of inhabitants with average, high or very high PSVI” and crude stillbirth presented positively and weak correlation with “birth rates”. However, Pearson correlation coefficients do not consider the spatial effect, so values cannot be adjusted by the neighborhood matrix. Therefore, Lee coefficients, that incorporate data spatial structure, were calculated, and indicated that the “proportion of inhabitants with average, high or very high PSVI”, “mortality rates in women of childbearing age” and “proportion of adolescent mothers” were most strongly associated with crude stillbirth rates.
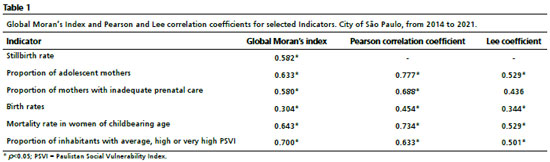
Thus, Lee coefficients demonstrate that higher social vulnerability, higher mortality rates in women of childbearing age and higher proportion of adolescent mothers are associated with higher stillbirth rates, considering the cutoff point of 0.50, this value is arbitrary and can be chosen by the researchers (Table 1).
DiscussionThis study identified the areas with higher stillbirth rates and indicated that the vulnerability index PSVI, adolescent mothers and mortality in women of childbearing age were the most correlated to stillbirth rates amongst other indicators. This study was able to identify significant differences between crude stillbirth rates between 2014 and 2021 with the respective values of 7.65 and 8.40 stillbirths/1000 births, indicating a slight increasing trend over the years. Therefore, about fetal death, a decrease in behavior and number of cases over time in the city of São Paulo has occurred.
The city of São Paulo has a public policy focused on pregnant women, based on the Network for Protection of Paulistan Mother, since 2006, as a strategy of the SUS. This program provides health care and support to all pregnant women in the municipality from the pregnancy onset, guaranteeing a minimum of seven prenatal consultations, as well as consultations during childbirth and the puerperium, up to the second year of the child’s life
18. Although the coverage of actions and health services concerning pregnant women has increased over time, some more peripheral districts in the municipality still present high proportions of inadequate prenatal care, with fewer than seven prenatal visits, corroborating the findings reported herein.
19Studies reporting stillbirth in the spatial context have been underexplored in Brazil, and few studies were identified in the examined literature. The studies focusing on perinatal mortality without separating the fetal component found evidence of spatial dependence in 645 areas of the state of SP and in 63 areas of the city of Salvador.
10 Silva
et al.
11 identified in Recife, state of Pernambuco, areas with significant social inequalities and lack of access to prenatal care. Silva
et al.
12 identified correlation between stillbirth rates and social vulnerability in the state of Pernambuco.
In the present study, crude stillbirth rates were correlated positively and moderately with social vulnerability, adolescent mothers, inadequate prenatal care and mortality rate in women of childbearing age. The assessed social vulnerability indices in the municipality worsened with increasing distance from the central region. This pattern was also observed in the proportion of adolescent mothers and mortality rate in women of childbearing age. The more peripheral the residence area, the greater the social vulnerability and the higher the proportion of adolescent mothers and mortality rate in women of childbearing age. Consequently, the risk of stillbirths among pregnant residents increases in these areas.
Consistently, it has been observed that a previous spatial analysis for health indicators showed that in the city of São Paulo, the pattern of clusters relating the central-periphery effect is related in several outcome: births, differences in maternal, gestational, labor and newborn characteristics;
20 social vulnerability and the proportion of mothers under 18 years old, low maternal education and fewer prenatal visits, spatial correlations between the proportion of adolescent mothers and socioeconomic status for births in the city of São Carlos, located in state of SP; higher risk for fetal deaths due to avoidable causes and social deprivation,
21 The social deprivation was associated to fetal and infant mortality, in the city of Recife.
22 The proportion of school-age children with dental caries increases with increasing distance from the central region towards the peripheral areas of the city, as well as with the average family income, unemployment rate, household overcrowding and the income distribution inequality index.
23 The spatial correlation of socioeconomic factors and other health outcomes were also found in some studies. In the state of São Paulo, spatial patterns of mortality of low birth weight infants have been analyzed, revealing a correlation with maternal and socioeconomic determinants.
24 Similarly, Andrade
et al.
25 examined the impact of socioeconomic factors and health determinants on preterm birth rates across Brazil, identifying higher preterm birth rates in rural and less affluent areas. All these studies showed the presence of socioeconomic differentials in spatial distribution and possible associations with health outcomes. Understanding how these dynamics influence health outcomes could provide a better management of the health services. Exploratory analyses are a fundamental part of the study and are a basis for analysis as spatial-temporal regressions. Methods to deal with a larger number of indicators that jointly associate to the outcome can be implemented as a part of the exploratory analysis. A better selection of variables is also desired, even though it is hard to establish a cutoff point for the correlation values.
Prenatal care is the indicator that presented the lowest correlation coefficient in our study. Despite this result, several studies have related fetal deaths to inadequate or absent prenatal care in Brazil,
26,27 indicating failures in health assistance, such as absence, inadequacy and failure to attend consultations. These findings highlight the challenge faced by neonatologists, obstetricians, and the public sector in improving the quality and conditions of care regarding gestation, delivery, and newborn care through public policies.
28 A modern antepartum and intrapartum care must be implemented including fetal monitoring, especially in low-income settings,
29 in which the areas identified could be more straightforward considered to receive such improvements.
The crude and Bayesian estimates (both global and local) demonstrated a high degree of similarity, indicating consistent patterns of identification of the clusters. The Global Moran’s index and Global Geary’s coefficient showed evidence of spatial association, while the LISA identified a low-risk cluster in the Western region of the municipality, and a high-risk cluster in the Eastern region of the municipality. The Moran scatterplot classified 40 districts as HH clusters, located in extreme and peripheral regions, with a concentration of eastern districts, while LL clusters concentrated 39 districts in the central region. The LISA results corroborated the Moran’s index. Of the eight districts presenting the highest overall Bayesian stillbirth rates (Cidade Tiradentes, Iguatemi, Vila Jacuí, Itaquera, Itaim Paulista, Socorro, Perus and Lajeado), all of them belong to the high-risk cluster, however, three districts did not present a significant standardized LISA index. Amongst the 8 lowest-risk districts (Lapa, Itaim Bibi, Vila Mariana, Perdizes, Moema, Carrão, Vila Leopoldina and Jardim Paulista), all of them belong to the low-risk cluster, but Carrão district, in the Southeast zone, did not present a significant standardized LISA index. These results also indicate convergence of all the performed analyses.
The limitations of the present study include the use of secondary data and, even with the use of indicators from the districts, instead of clustering districts, we still could not ensure homogeneity. Another issue is the underreporting of stillbirths that could affect the rates. In poorest parts of Brazil, underreporting was 10% and this percentage was higher in smaller municipalities.
30 The Network of Protection for the Paulistan Mother could minimize this effect by providing access to hospital for the mothers with fetal loss, although we did not find information about the underreporting estimation in the city. The concept of death may be classified by different criteria according to country or region, restricting comparisons of the obtained result with other countries. On the other hand, this study demonstrated the impact of indicators on stillbirth and their relation to spatial inequalities. The living conditions of the population contributes to the disparity of stillbirth in the city of São Paulo, and this study indicates some important indicators for the public health service managers, especially in regions presenting high risk for fetal death.
The findings of this study, based on an exploratory spatial analysis, indicated that the PSVI, adolescent mothers and mortality in women of childbearing age were the most correlated to stillbirth rates, amongst other indicators. The identification of these areas may be used by the public health services managers to understand how health services are distributed and which interventions might reduce stillbirth rates in these regions. The exploratory spatial analysis as presented here can contribute to the selection of variables in further analysis.
References1. Chou VB, Daelmans B, Jolivet RR, Kinney M, Say L. Ending preventable maternal and newborn mortality and stillbirths. Lancet. 2021; 398 (10303): 675-708.
2. United Nations Children’s Fund (UNICEF). Never forgotten: The situation of stillbirth around the globe. Report of the United Nations Inter-agency Group for Child Mortality Estimation 2022. New York: UNICEF; 2023. [
Internet]. [access in 2024 Aug 20]. Available from:
https://data.unicef.org/resources/never-forgotten-stillbirth-estimates-report/3. Hug L, You D, Blencowe H, Mishra A, Wang Z, Fix MJ,
et al. Global, regional, and national estimates and trends in stillbirths from 2000 to 2019: a systematic assessment. Lancet. 2021; 398 (10302): 772-85.
4. Mirbaha-Hashemi F, Tayefi B, Rampisheh Z, Tehrani-Banihashemi A, Ramazani M, Khalili N,
et al. Progress towards Every Newborn Action Plan (ENAP) implementation in Iran: obstacles and bottlenecks. BMC Pregnancy Childbirth. 2023; 23 (1): 123.
5. Andrews K, Bourroul MLM, Fink G, Grisi G, Ferrer APS,
et al. Time to change focus? Transitioning from higher neonatal to higher stillbirth mortality in São Paulo State, Brazil. PLoS One. 2017; 12 (12): 1-13.
6. Corrêa TA, Lima EPO, Silva AT, Barreto LS, Silva RPP, Braga CH,
et. al. Principais fatores de risco associados ao óbito fetal: revisão integrativa. Rev Elet Acervo Saúde. 2021; 13(2): e6407.
7. Canutto IMB, Oliveira CM, Silva APSC, Bonfim CV. Spatial dynamics of fetal mortality and the relationship with social vulnerability. J Perinat Med. 2021; 50 (6): 645-52.
8. Marques LJP, Silva ZP, Moura BLA, Francisco RPV, Almeida MF. Intra-urban differentials of fetal mortality in clusters of social vulnerability in São Paulo Municipality, Brazil. Sci Rep. 2021; 11: 24256.
9. Venâncio T, Tuan TS, Vaz FPC, Nascimento LFC. Spatial approach of perinatal mortality in São Paulo State, 2003-2012. Rev Bras Ginecol Obstet. 2016; 38 (10): 492-8.
10. Nascimento RCS, Costa MCN, Braga JU, Natividade MS. Spatial patterns of preventable perinatal mortality in Salvador, Bahia, Brazil. Rev Saúde Pública. 2017; 51: 73.
11. Silva MCL, Oliveira CM, Silva APSC, Bonfim CV. Spatial patterns of fetal mortality: scenario before and after the implementation of surveillance. Rev Bras Saúde Matern Infant. 2021; 21 (3): 889-95.
12. Silva MO, Macedo VC, Canuto IMB, Silva MC, Costa HVV, Bonfim CV. Spatial dynamics of fetal mortality and the relationship with social vulnerability. J Perinat Med. 2021; 50 (6): 645-52.
13. São Paulo. Secretaria da Saúde do Município de São Paulo. Mortalidade e Nascidos Vivos da Cidade de São Paulo – Tabnet. São Paulo: Prefeitura de São Paulo; 2024. [Internet]. [access in 2024 Aug 20]. Available from:
https://capital.sp.gov.br/web/saude/tabnet/14. São Paulo. Fundação SEADE. Metodologia do IPVS. São Paulo: Fundação SEADE; 2013. [Internet]. [access in 2024 Aug 20]. Available from:
http://ipvs.seade.gov.br/view/pdf/ipvs/metodologia.pdf15. São Paulo. Geosampa. São Paulo: Prefeitura de São Paulo; 2024. [Internet]. [access in 2024 Aug 20]. Available from:
http://geosampa.prefeitura.sp.gov.br/PaginasPublicas/_SBC.aspx16. Anselin L. An Introduction to Spatial Data Science with GeoDa: Volume 1: Exploring Spatial Data. Boca Raton: Chapman and Hall/CRC Press; 2024.
17. Bivand RS, Pebesma E, Gómez-Rubio V. Applied Spatial Data Analysis with R. 2
nd ed. New York: Springer; 2013.
18. São Paulo. Relatório Rede de Proteção à Mãe Paulistana Também é Rede Cegonha. Convênio 004/2012. Jan 2009-Mar 2015. São Paulo: Secretaria Municipal da Saúde; 2015.
19. São Paulo. Secretaria da Saúde do Município de São Paulo; Instituto Via Pública. Atlas da saúde da cidade de São Paulo. São Paulo: Secretaria Municipal de Saúde e Instituto Via Pública; 2011. [Internet]. [access in 2024 Aug 20]; 182 p. Available from:
https://www.prefeitura.sp.gov.br/cidade/secretarias/upload/saude/arquivos/publicacoes/atlas_da_saude_da_cidade_de_sao_paulo_2011.pdf20. Santos PC, Silva ZP, Neto FC, Alencar GP, Almeida MF. Diferenciais dos aglomerados de nascidos vivos no Município de São Paulo, Brasil, 2010. Cad Saúde Pública. 2018; 34 (6): e00156416.
21. Ferreira RA, Ferriani MGC, Mello DF, Carvalho IP, Cano MA, Oliveira LA. Spatial analysis of social vulnerability of teenage pregnancy. Cad Saúde Pública. 2012; 28 (2): 313-23.
22. Bonfim CV, Silva APSC, Oliveira CM, Vilela MBR, Freire NCF. Spatial analysis of inequalities in fetal and infant mortality due to avoidable causes. Rev Bras Enferm. 2020; 73 (Suppl. 4): e20190088.
23. Antunes JLF, Frazão P, Narval PC, Bispo CM, Pegoretti T. Spatial analysis to identify differentials in dental needs by area-based measures. Community Dent Oral Epidemiol. 2022; 30 (2): 133-42.
24. Rodríguez EYA, Rodríguez ECA, Marins FAS, Silva AF, Nascimento LFC. Spatial patterns of mortality in low birth weight infants at term and its determinants in the State of São Paulo, Brazil. Rev Bras Epidemiol. 2023; 26: e230034.
25. Andrade L, Kozhumam AS, Rocha TAH, Almeida DG, Silva NC, Queiroz RCS,
et al. Impact of socioeconomic factors and health determinants on preterm birth in Brazil: a register-based study. BMC Pregnancy Childbirth. 2022; 22 (1): 872.
26. Fonseca SC, Coutinho ESF. Risk factors for fetal mortality in a maternity hospital of the Unified Health System, Rio de Janeiro, Brazil: a case-control study. Cad Saúde Pública. 2010; 26 (2): 240-52.
27. Almeida MF, Alencar GP, Novaes HMD, França Jr I, Siqueira AAF, Campbell OMR,
et al. Risk factors for antepartum fetal deaths in the city of São Paulo, Brazil. Rev Saúde Pública. 2007; 41 (1): 35-43.
28. Barros PS, Aquino EC, Souza MR. Fetal mortality and the challenges for women’s health care in Brazil. Rev Saúde Pública. 2019; 53: 71.
29. Goldenberg RL, Saleem S, Pasha O, Harrison MS, McClure EM. Reducing stillbirths in low-income countries. Acta Obstet Gynecol Scand. 2016; 95: 135-43.
30. Barbeiro FMS, Fonseca SC, Tauffer MG, Ferreira MSS, Silva FP, Ventura PM,
et al. Fetal deaths in Brazil: a systematic review. Rev Saúde Pública. 2015; 49: 1-15.
Author’s contributionNahas AK: conceptualization (Equal), Data curation (Equal), Formal analysis (Equal), Funding acquisition (Equal), Investigation (Equal), Methodology (Equal), Project administration (Equal), Resources (Equal), Software (Lead), Supervision (Equal), Validation (Equal), Visualization (Equal), Writing – original draft (Lead), Writing – review & editing (Equal).
Alencar GP: conceptualization (Equal), Data curation (Equal), Formal analysis (Equal), Funding acquisition (Equal), Investigation (Equal), Methodology (Equal), Project administration (Equal), Resources (Equal), Software (Supporting), Supervision (Equal), Validation (Equal), Visualization (Equal), Writing – original draft (Supporting), Writing – review & editing (Equal).
All authors approve the final version of the article and declare no conflicts of interest.
Received on May 7, 2022
Final version presented on September 11, 2024
Approved on Septemberm 13, de 2024
Associated Editor: Sheyla Costa
 ; Gizelton Pereira Alencar 2
; Gizelton Pereira Alencar 2