ABSTRACT
OBJECTIVES: to analyze the spatio-temporal distribution of maternal mortality in Brazil from 2000 to 2019.
METHODS: an ecological, longitudinal study of space-time analysis of maternal deaths in Brazil from 2000 to 2019, using the 450 health regions as the spatial unit. Data available from Datasus were used. Analyses were conducted using Satscan v9.7 software, considering the discrete Poisson probability model.
RESULTS: five clusters of high maternal mortality were identified, predominantly in the North and Midwest regions, as well as in the state of Rio de Janeiro and parts of the Northeast. Five low-risk clusters were identified, mainly along the northeastern coast and in states in the South and Southeast. Temporal analysis revealed a low-risk cluster from 2000 to 2007 (RR=0.92; p<0.001), indicating significant advances in maternal health during this period.
CONCLUSIONS: the North region of the country showed high MMR values, concentrating high-risk clusters in the spatiotemporal analysis, with high MMR between 2000 and 2009, showing a correlation of maternal mortality with the country's socioeconomic inequalities.
Keywords:
Maternal mortality, Spatio-temporal analysis, Global health strategies
RESUMO
OBJETIVOS: analisar a distribuição espaço-temporal da mortalidade materna no Brasil nos anos de 2000 a 2019.
MÉTODOS: estudo ecológico, longitudinal, de análise espaço-temporal dos óbitos maternos no Brasil, de 2000 a 2019, utilizando como unidade espacial as 450 regiões de saúde com dados disponíveis no Datasus. As análises foram feitas com o software Satscan v9.7, considerando o modelo de probabilidade discreto de Poisson.
RESULTADOS: foram identificados cinco clusters de alta mortalidade materna, predominantemente nas regiões Norte e Centro-Oeste, além do estado do Rio de Janeiro e partes do Nordeste. Cinco clusters de baixo risco foram identificados, principalmente na costa nordestina e em estados do Sul e Sudeste. A análise temporal revelou um cluster de baixo risco de 2000 a 2007 (RR=0.92; p<0.001), indicando avanços significativos na saúde materna durante esse período.
CONCLUSÕES: a região Norte do país apresentou altos valores de RMM, concentrando clusters de alto risco na análise espaço-temporal, com altas RMM entre 2000 e 2009, mostrando uma correlação da mortalidade materna com o perfil de desigualdades socioeconômicas do país.
Palavras-chave:
Mortalidade materna, Análise espaço-temporal, Estratégias de saúde globais
IntroductionMaternal mortality is a persistent and crucial challenge for public health in Brazil. This country has complex dynamics that affect women’s health during pregnancy, delivery and postpartum. In spite of the significant advances in healthcare in the last decades, maternal mortality still being a main concern.
1The 10
th Revision of the International Classification of Diseases (ICD-10) defines maternal death as “death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and the site of the pregnancy, from any cause related or aggravated by the pregnancy or its management, but not from accidental or incidental causes”.
2 The main epidemiological indicator used to measure this datum is the Maternal Mortality Ratio (MMR), which assess the risk of death in a single pregnancy or birth.
3The comprehension of the factors that contribute to this problem, as well as the identification of effective solutions, are necessary to grant health and wellbeing of Brazilian mothers. For such, several strategies were adopted to enhance the registry of deaths in Brazil, including the creation of Commissions of Investigation of Perinatal and Maternal Mortality in state and municipal health secretariats, by the Ministry of Health (MS – Portuguese acronym) from 1994 onwards. Such measures aimed to include information related to pregnancy, abortion, delivery and puerperium in the national death certificate and in the Information System on Mortality (SIM – Portuguese acronym), as well as the mandatory notification of maternal death within 24 hours after death. These efforts, carried out by the Brazilian Ministry of Health, with participation of National Commissions, state health secretariats and State and Municipal Committees for Maternal Death Surveillance, have been effective in reducing maternal mortality in the last years. However, the COVID-19 pandemic onset in 2020 had and still having significant impact in this mortality indicator.
4,5A study, which used data from SIM, assessed maternal deaths in the period from March 2020 to May 2021 by means of generalized additive models. The results revealed a significant 70% increase of deaths, regardless of the region of the country. The regions North, Northeast and South registered such increase in all age groups, which stood out as a consistently elevated phenomenon.
6 Other studies indicated that eight out of ten maternal deaths by COVID-19 registered worldwide occurred in Brazil.
4 Events of great magnitude, such as COVID-19 pandemic, highlight the vulnerabilities of health systems and increase the gaps in the access to services, resulting in an increase of the MMR.
7,8The emergency of this new threat to maternal health highlights the imperious need for a continuous analysis of factors subjacent to maternal mortality. These factors comprise a group of variables, including advanced maternal age, lower levels of schooling, occupation, reduced frequency of prenatal consultations, among other critical determinants.
9,10The search for effective solutions to mitigate these deaths are imperative for developing countries. Many studies have been limited to percentage comparisons and not using the most adequate indicator: the MMR.
Moreover, the analysis of spatio-temporal distribution of maternal mortality in Brazil is still underexplored, in spite of its potential in clarifying the determinants of regional variations on these events. Due to the regional diversity of the country, the use of health regions is essential to comprehend maternal mortality, allowing identifying standards and specific challenges in different areas, to direct public policies in a more effective manner, to assess specific interventions and mobilize local actions to improve maternal assistance. In this way, the objective of this study was to assess regional differences in the distribution of maternal deaths in Brazil, by means of the spatio-temporal analysis of MMR between 2000 and 2019.
MethodsThe main epidemiological indicator used to measure this datum is the MMR, defined as the number of maternal deaths in a population divided by the number of live births, expressed by 100,000 in a giventime period and space.
11We conducted an epidemiological cross-sectional study, of ecological type, with analysis of spatial and temporal clusters, using secondary data available at SIM and at the Live Birth Information System (SINASC – Portuguese acronym), both accessed with the information platform of the Ministry of Health: Datasustabnet. An ecological study aims at the comparative analysis between groups, and not individuals. Due to this reason, there is absence of detailed information at individual level about the joint distribution of variables within these groups. The variables in ecological studies generally include aggregate measures, such as environmental data, or more global and embracing measures.
12 Data were accessed in the “vital statistics” icon, selecting the option “Mortality – 1996 to 2019m by ICD-10” and “Live births – 1994 to 2019”. Data concerning maternal death were collected in the topic “Death of women of childbearing age and maternal deaths”.
The spatial units of analysis selected were the Health Regions (REGS – Portuguese acronym). The decree number 7508, from July 28, 2011, which looks after the organization of the Unified Health System (SUS – Portuguese acronym), defines health region as “a geographic continuous space composed of clusters of neighboring municipalities, delimited from shared cultural, economic and social identities and communication and transport structure, aiming to integrate organization, planning and execution of actions and health services.”
13 We then collected the coordinates corresponding to the centroids of each REGS in the form of decimal degrees of latitude and longitude from the Brazilian Institute of Geography and Statistics – IBGE (Portuguese acronym), resulting in 450 REGS in the entire national territory, distributed into 46 in the North, 133 in the Northeast, 38 in the Midwest Region, 165 in the Southeast Region and 68 in the South.
The minimum analysis units were the REGS. These regions were selected due to their relevance for the analysis of maternal mortality, since they reflect the organization of the health system and the geographic distribution of health services and they may vary significantly in extension and complexity.
The MMR calculation uses as numerator the number of maternal deaths per location of residence, also as denominator the number of live births per location of residence of the mother, generating a ratio of deaths per 100 000 live births, per year, per health region.
We conducted a broad analysis of maternal mortality in Brazil using the technique of spatial, temporal and spatio-temporal scanning. We used the SaTScan sv9.720 software to identify clusters of health regions with maternal mortality ratio above or under the expected. These primary clusters, in which maternal mortality had less probability of being random, were identified and assessed based on probability values. Moreover, secondary clusters were identified in spatial and spatial-temporal analyses. We used the “relative risk” (RR) to assess the susceptibility of different areas to maternal mortality.
14Values above 1 indicate clusters with a mortality ratio above the expected (called risk cluster), whereas values under 1 indicate clusters with observed mortality ratios under the expected (called protection clusters). For the assessment of significance to the level of
p<0.05 in the model, we used the Monte Carlo simulation. Besides the spatial and spatio-temporal analyses, we performed purely temporal analyses, with annual precision, aiming to identify significant temporal trends, also using
p<0.05.
14ResultsTable 1 shows the distribution of the absolute number of deaths, the percentage and the MMR in Brazilian regions. It is noted that the North region demonstrates a mean MMR of 107.06 deaths/100,000 LB, the highest within the five regions.
The purely spatial analysis, performed posteriorly with an adjustment of the circular window to 10%, found ten clusters with statistical significance (
p<0.05), five clusters with MMR higher than expected (high-risk) and five clusters with MMR lower than expected (low risk), represented in the maps in Figure 1. The first high-risk cluster, named cluster A, comprises the states of Maranhão and Piauí, the Northeast of Tocantins and West of Ceará; it was found a ratio deaths found/expected of 1.47 and Relative Risk (RR) of 1.54,
p<0.001. The second high-risk cluster (A) comprises most of the state of Rio de Janeiro and the Southeast of Minas Gerais; ratio deaths found/expected of 1.31 and RR of 1.35,
p<0.001. The third high-risk cluster (C) comprises a significant part of the state of Bahia and Sergipe and the Northeast of Minas Gerais; with a ratio of deaths found/expected of 1.19 and RR of 1.22,
p<0.001. The fourth high-risk cluster (D) comprises the entire state of Mato Grosso do Sul and the South of Mato Grosso, with ratio of deaths found/expected of 1.21 and RR of 1.21,
p<0.001.
The low risk clusters found were: the first (F), located in the Northeast of the state of São Paulo and South of Minas Gerais, comprising the capital São Paulo, the municipalities of Campinas and Ribeirão Preto; ratio of deaths found/expected of 0.65 and RR of 0.62,
p<0.001. The second cluster (G), with smaller geographic scope, is also located in the state of Minas Gerais, however in the central region, comprising the capital Belo Horizonte and neighboring municipalities; this location had a ratio of deaths found/expected of 0.66 and RR of 0.74,
p<0.001.The third cluster (H) is located in the South of the country, comprising the states of Santa Catarina and Rio Grande do Sul and the South of the state of Paraná, including the capital Curitiba; the ratio deaths found/expected was 0.76 and RR of 0.74,
p<0.001. The fourth low risk cluster (I), comprised a really small area of São Paulo, specifically the municipality of São Bernardo do Campo, ratio of deaths found/expected 0.81 and RR of 0.8,
p<0.001. Finally, the fifth low risk cluster (J) is located in the Northeast of Brazil, near the coastline, comprising the East portion of Pernambuco, Paraíba, Alagoas and Rio Grande do Norte, where the capitals and their neighboring municipalities are located; with a RR of 0.9 and ratio of deaths found/expected of 0.9,
p<0.001. (Table 2).
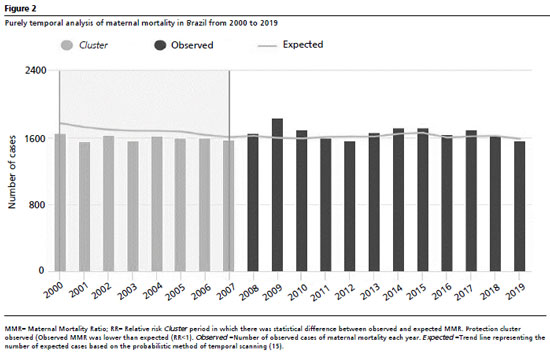
The purely temporal analysis (Figure 1) found only one cluster with statistical significance, situated in the period from 2000 to 2007, with mean MMR of 53.5 deaths/100 000 live births, ratio of cases expected/found of 0.95 and RR of 0.92,
p<0.001. The spatio-temporal analysis found seven clusters (Table 3), all with statistical significance and
p<0.001, six clusters having high-risk and only one with low risk, demonstrated in the maps of Figure 1. The high-risk clusters found were the following: the first cluster (cluster 1) comprises the states of Maranhão, Piauí and Ceará, encompassing the period from 2000 to 2009, presented a relation of number of cases found/expected of 8.77 and RR of 9.4,
p<0.001. The second cluster (2) included the state of Rio de Janeiro, the Southeast of Minas Gerais and the Northeast of São Paulo, encompassing the period from 200 to 2009, with a ratio of observed deaths/expected of 7.42 and RR of 7.84,
p<0.001. The third cluster comprises the North of the state of Minas Gerais, part of Espírito Santo and Bahia, also situated in the period from 2000 to 2009, with ratio of deaths found/expected of 6.95 and RR of 7.35,
p<0.001. The fourth cluster comprises the state of Paraná, part of Santa Catarina and North of Rio Grande do Sul, in the period from 2000 to 2006 , ratio of observed deaths/found of 10.53 and RR of 10.91,
p<0.001. The fifth cluster (5) comprises the states of Amazonas and Rondônia, part of Amapá, Pará and Mato Grosso, in the period from 2000 to 2009, with aratio of observed cases/found of 6.38 and RR of 6.66,
p<0.001. The sixth cluster (6) found has a significantly smaller geographic scope, located in São Paulo, in the municipality of São Bernardo do Campo, in the period from 2000 to 2009, with a ratio of cases found/expected of 4.84 and RR of 5.0,
p<0.001. The only low risk cluster (7) found in the spatio-temporal analysis is located in the Northeast of São Paulo, encompassing the capital and the municipalities of Campinas and Ribeirão Preto, in the period from 2013 to 2019, with ratio of observed/expected cases of 0.31 and RR of 0.30,
p<0.001.
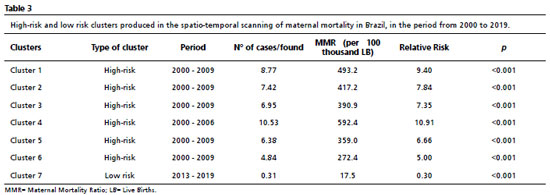
Figure 1 highlights the high-risk clusters in the first image, that is, the locations where the calculated MMR was higher than expected. Despite the similarity of distribution of these clusters, there is no perfect overlap comparing the localization of clusters. This difference (Figure 1) is more evident in the South region, which in the purely spatial analysis, presents low risk clusters, and in the spatio-temporal analysis, concentrates high-risk clusters. The North region of the country presented high values of MMR and concentrated high-risk clusters both in spatial analysis and spatio-temporal analysis, with high MMR from 2000 and 2009. The Midwest region concentrated high-risk clusters for maternal mortality between 2000 and 2019 in our study. Figure 2 demonstrates a thorough analysis of the period between 2000 and 2019, focused on maternal mortality in Brazil. We observed that between 2000 and 2007, there was a notable decrease of the relative risk of maternal mortality (relative risk <1), suggesting a period of protection and significant improvements in maternal health during this interval.
Maternal mortality is a crucial indicator of the quality of reproductive health in the country and an important reflection of social and economic inequalities. In Brazil, the spatio-temporal analysis of maternal mortality between 2000 and 2019 reveals both advances and persistent challenges. Between 2000 and 2019, Brazil experienced a decrease in MMR. However, this reduction was not uniform in the entire country. More developed regions, such as Southeast and South, presented lower MMRs, whilst less developed regions, such as North and Northeast, still had significant challenges. The Northeast and Southeast regions are responsible for the highest percentages of maternal deaths that occurred in Brazil, although the region with the highest MMR in the period is the North region. The World Health Organization (WHO) classifies regions according to the MMR values, into “recommended”, “low”, “moderate”, “high” and “extremely high”. None of Brazilian regions presented a MMR in the level recommended by WHO during the period, that is, between 20 and 35 deaths/100 000 live births. In spite of that, all regions stood in the “low” classification, that is, a MMR between 20 and 99; except for North region, whose MMR is “moderate”.
3This decrease in the country’s MMR may be associated with improvements in maternal health during this period, a progress related to several policies and public health programs. The Program of Humanization of Prenatal and Birth (PHPN – Portuguese acronym), for example, emphasized the importance of maternal deaths related to high-risk pregnancy.
16 Mota
et al.
17 demonstrated that the dissemination of Maternal Mortality Committees, the National Policy of Integrative Care to Women’s Health (PNAISM – Portuguese acronym) and the Stork Network influenced the decrease of the MMRs in Brazil in the beginning of the decade, mainly for women from 30 to 49 years old, with a less significant reduction for younger women.
17 Moreover, the expansion of access to health services, such as SUS (Portuguese acronym for Unified Health System), played an essential role in the improvement of maternal health indicators.
However, some significant challenges persist for the reduction of maternal mortality in Brazil. First, regional inequalities are still a critical problem. Poorer and remote regions still experience impairments in the access to health services of quality and in the qualification of health professionals, which contributes to higher maternal mortality ratios.
18 An example of this challenge is represented by the linking of pregnant women to a maternity hospital, which is provided for by law since 2005, although the compliance with this law is not reachable for all Brazilian women, mainly in poorer regions, such as the North and Northeast.
19A significant limitation of this study refers to the quality and scope of death registries in Brazil. However the SIM was established in 1976 and had achieved a coverage of 82% up to 1999, challenges related to regional variations of coverage persist. The introduction of the term “garbage code” in the national literature reflects the concerns with misclassification of deaths, especially in the maternal mortality area, hindering the clarity and accuracy of data.
20 Although it is relevant to highlight recent improvements, such as the establishment of the Commissions of Surveillance of Perinatal and Maternal Mortality, the inequalities and imprecisions persist, mainly at a regional level.
The occurrence of a maternal death is profoundly tragic and demands meticulous investigations. Errors such as the garbage codes and other problems associated with underdiagnosis and under-registration may lead to underreporting, resulting in a distorted representation of the real magnitude of the challenges to maternal health.
21 Being aware of and approaching these limitations is essential for the reformulation of effective preventive strategies.
The scarcity of studies on determinants of maternal mortality in the North region of the country, which concentrates the highest MMRs and even with rates extremely higher than those recommended by WHO, demonstrates the importance of deepening the investigation on the subject. Several studies demonstrated the spatial correlation between maternal mortality, the Social Vulnerability Index (IVS – Portuguese acronym) and income inequality.
22 The North region of the country presented, between 2000 and 2010, an IVS in the scale of high and very high. From 2011 up to 2013, the vulnerability started to decrease, stabilizing in “average”.
23The finding of high-risk clusters for maternal mortality in the North region of Brazil may be intrinsically related to adversities associated with income distribution and precariousness of infrastructure in that location compared to other regions of the country. Moreover, geographic characteristics peculiar to the North region stand out as additional challenges to the access to health services, among other factors that contribute to this problem. This occurs because socioeconomic inequalities play a preponderant role in both quality of and access to health services, which becomes more evident when maternal health is analyzed. Women that are part of more vulnerable socioeconomic strata often face significant barriers to access healthcare services of quality during pregnancy and delivery period. It is alarming to observe that MMR is considerably higher for black and indigenous women compared to white women. It is worth highlighting that this inequality is not solely related to socioeconomic issues, but is strongly linked to challenges perpetuated by the structural racism that is rooted in the health system.
5,24Another important question to be considered is the distribution of race/color in Brazil. According to what the National Household Sample Survey (PNAD – Portuguese acronym) of 2022, published by the Brazilian Institute of Geography and Statistics (IBGE), the population self-declared as black or brown is predominant in the North and Northeast regions, corresponding to 78.4% and 73.9%, respectively. In comparison, the South region has 26.3% of its population identified as such, whilst the Southeast has 49.9%, and the Midwest, 62.6%. Moreover, it is important to highlight that the North region houses 44.48% of the indigenous population of Brazil.
25 States such as Mato Grosso and Maranhão also have a significant concentration of indigenous people. This demographic distribution, with the predominance of groups historically more vulnerable in the North and Northeast regions, may be one of the factors that explain the inequalities of MMR between the different regions of the country.
Albuquerque
et al.
26 characterized the health regions of Brazil according to a typology that considered the level of socioeconomic development and the offer and complexity of health services. The Midwest region demonstrated average and high levels of socioeconomic development, however they kept a low offer and complexity of local health services. The South and Southeast regions presented, in the same study, higher concentration of areas of high socioeconomic development and average to high concentrations of local health services, being also consistent with our findings, since such regions, mainly the state of São Paulo, concentrated the clusters of the lowest risk of maternal death in the country.
26In order to overcome these challenges, Brazil needs to keep investments in maternal health policies that contemplate the needs of more vulnerable populations. This includes improving the access to health services of quality, qualifying health professionals and promoting sexual and reproductive education.
17Besides, the fight against racism and discrimination in the health system is essential to reduce inequalities in maternal mortality.
In spite of the relevance of this subject, the scarcity of broad studies on maternal mortality that compare the different regions of Brazil is evident. In 2011, a study conducted by Morse
et al.
27 clarified this gap with a scientific literature review focused on maternal mortality in the country in the last three decades. The results revealed that most articles published on the team concentrated significantly the Southeast region of Brazil, with predominance of descriptive approaches.
27 This predominance in the scientific production limited to one region, mainly of a strictly descriptive nature, does not reflect the complexity and diversity of the panorama of maternal mortality in the entire country. It is particularly concerning the lack of studies focused on the analysis of MMR in the North region of the country, since this region consistently has higher values for this indicator than the national averages.
28 This scarcity of surveys dedicated to comprehend the particularities and challenges of the North region highlights the imperious need for promoting broader and more detailed discussions on this subject.
The third Sustainable Development Goal, Good Health and Well-being, preconizes the reduction of maternal mortality in countries where high rates of deaths related to delivery and puerperium are still being a severe public health problem. Brazil is one of these countries where maternal mortality is still unacceptably high, despite its causes being mostly avoidable when screened early and treated adequately.This article aimed to contribute to the available literature on the theme by means of a spatio-temporal analysis of the distribution of these deaths in the country in the last 20 years, using public data, easily accessible. We found a distribution of clusters of high-risk for maternal mortality with predominance in the North region, part of the Northeast and Midwest and low risk clusters in the South and Southeast regions and in the Northeast coastline. Such distribution is consistent with regional inequalities peculiar to the country, in the income distribution and access to health services. We even found a temporal cluster with MMR lower than expected in the first years of the analyzed period (2000-2007), which may reflect the impact of policies established in the beginning of the century. It is important to highlight that surveys that assess maternal mortality in Brazil are and will be even more essential in the next years, especially considering the impacts of Covid-19 pandemics in maternal mortality.
References1. Alkema L, Chou D, Hogan D, Zhang S, Moller AB, Gemmill A, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet. 2016 Jan; 387 (10017): 462-4.
2. Organização Mundial da Saúde (OMS). Classificação Internacional de Doenças - décima revisão (CID-10). São Paulo: Edusp; 1998.
3. World Health Organization (WHO). Trends in maternal mortality: 1990 to 2010. [Internet]. 2012. 59 p. [access in 2023 Oct 30]. Available from:
https://iris.who.int/bitstream/handle/10665/44874/97892415%2003631_eng.pdf;jsessionid=ED47375350F26F6C137F9CFB0934AEC3?sequence=14. Souza ASR, Amorim MMR. Maternal mortality by COVID-19 in Brazil. Rev Bras Saúde Matern Infant. 2021 Feb; 21 (Suppl. 1): 253-6.
5. Góes EF, Ferreira AJF, Ramos D. Racismo antinegro e morte materna por COVID-19: o que vimos na Pandemia? Ciên Saúde Colet. 2023 Sep; 28 (9): 2501-10.
6. Orellana J, Jacques N, Leventhal DGP, Marrero L, Morón-Duarte LS. Excess maternal mortality in Brazil: Regional inequalities and trajectories during the COVID-19 epidemic. Sichieri R, editor. PLoS One. 2022 Oct; 17 (10): e0275333.
7. Andreucci CB, Knobel R. Social determinants of COVID-19-related maternal deaths in Brazil]. Lancet Regional Health - Americas. 2021 Nov; 3: 100104.
8. Long S, Loutfi D, Kaufman JS, Schuster T. Limitations of Canadian COVID-19 data reporting to the general public. J Public Health Policy. 2022 Jun; 43 (2): 203-21.
9. Feitosa-Assis AI, Santana VS. Occupation and maternal mortality in Brazil. Rev Saúde Pública. 2020 Jul; 54: 64.
10. Scarton J, Thurow MRB, Ventura J, Silva DN, Perim LF, Siqueira HCH. Mortalidade materna: causas e estratégias de prevenção. Res Soc Dev. 2020 Mar; 9 (5): e67953081.
11. Calvert C, John J, Nzvere FP, Cresswell JA, Fawcus S, Fottrell E, et al. Maternal mortality in the covid-19 pandemic: findings from a rapid systematic review. Glob Health Action. 2021 Oct; 14 (Sup. 1): 1974677.
12. Morgenstern H. Ecologic Studies in Epidemiology: Concepts, Principles, and Methods. Annu Rev Public Health. 1995; 16: 61-2.
13. Brasil. Decreto nº 7.508, de 28 de junho de 2011. Regulamenta a Lei no 8.080, de 19 de setembro de 1990, para dispor sobre a organização do Sistema Único de Saúde - SUS, o planejamento da saúde, a assistência à saúde e a articulação interfederativa, e dá outras providências. Brasília (DF): DOU de 29 de junho de 2011. [access in 2023 Oct 30]. Available from:
https://www.planalto.gov.br/ccivil_03/_Ato2011-2014/2011/Decreto/D7508.htm?msclkid=af8d8426d12111ec969c7954231d6d5a14. Souza ECO, Santos ES, Rosa AM, Botelho C. Varredura espaço-temporal para identificação de áreas de risco para hospitalização de crianças por asma em Mato Grosso. Rev Bras Epidemiol. 2019; 22: e190019.
15. Kulldorff MA. Spatial scan statistic. Commun Stat Theory Methods. 1997; 26 (6): 1481-96.
16. Leal MDC, Szwarcwald CL, Almeida PVB, Aquino EML, Barreto ML, Barros F, et al. Reproductive, maternal, neonatal and child health in the 30 years since the creation of the Unified Health System (SUS). Ciênc Saúde Colet. 2018 Jun; 23 (6): 1915-28.
17. Motta CT, Moreira MR. Will Brazil comply with the sdg 3.1 of the 2030 agenda? an analysis of maternal mortality, from 1996 to 2018. Ciênc Saúde Colet. 2021; 26 (10): 4397-409.
18. Souza JP. Mortalidade materna no Brasil: a necessidade de fortalecer os sistemas de saúde. Rev Bras Ginecol Obstet. 2011; 33 (10): 273-9.
19. Domingues RMSM, Dias MAB, Schilithz AOC, Carmo Leal M. Factors associated with maternal near miss in childbirth and the postpartum period: Findings from the birth in Brazil National Survey, 2011-2012. Reprod Health. 2016 Oct; 13 (Supl. 3): 115.
20. Marinho MF, França EB, Teixeira RA, Ishitani LH, Cunha CC, Santos MR, et al. Dados para a saúde: impacto na melhoria da qualidade da informação sobre causas de óbito no Brasil. Rev Bras Epidemiol. 2019; 22 (Suppl. 3): e190005.
21. Cardoso LSM, Teixeira RA, Ribeiro ALP, Malta DC. Premature mortality due to non-communicable diseases in Brazilian municipalities estimated for the three-year periods of 2010 to 2012 and 2015 to 2017. Rev Bras Epidemiol. 2021; 24.
22. Duarte EMS, Alencar ÉTS, Fonseca LGA, Silva SM, Machado MF, Araújo MDP,
et al. Maternal mortality and social vulnerability in a Northeast State in Brazil: a spatial-temporal approach. Rev Bras Saúde Matern Infant. 2020 Jun 1; 20 (2): 575-86.
23. Marguti BO, Santos RM. Avaliação continuada da vulnerabilidade social no Brasil: impressões e primeiros resultados do Índice de Vulnerabilidade Social (IVS) 2016-2017 [Internet]. Brasília (DF): Instituto de Pesquisa Econômica Aplicada (IPEA); 2019. [access in 2023 Oct 30]. Available from:
https://repositorio.ipea.gov.br/bitstream/11058/9666/1/BRUA21_Ensaio10.pdf24. Carvalho D, Meirinho D. O quesito cor/raça: desafios dos indicadores raciais de mortalidade materna como subsídio ao planejamento de políticas públicas em saúde. Rev Eletrôn Com Inform Inov Saúde. [Internet]. 2020 Sep 29; 14 (3). [access in 2023 Oct 7]. Available from:
https://www.reciis.icict.fiocruz.br/index.php/reciis/article/view/190525. Instituto Brasileiro de Geografia e Estatística (IBGE). Pesquisa Nacional por Amostra de Domicílios (PNAD). Brasília (DF): IBGE; 2022. [access in 2023 Oct 7]. Available from:
http://downloads.ibge.gov.br/downloads_estatisticas.htm?caminho=Trabalho_e_Rendimento/Pesquisa_Nacional_por_Amostra_de_Domicilios_continua/Mensal/Arquivos_ complementares_para_o_calculo_dos_indices_do_SNIPC/2022``[oaicite:0]``.
26. Albuquerque MV, Viana AL d’Ávila, Lima LD, Ferreira MP, Fusaro ER, Iozzi FL. Desigualdades regionais na saúde: mudanças observadas no Brasil de 2000 a 2016. Ciên Saúde Colet. 2017 Apr; 22 (4): 1055–64.
27. Morse ML, Fonseca SC, Barbosa MD, Calil MB, Eyer FPC. Mortalidade materna no Brasil: o que mostra a produção científica nos últimos 30 anos? Cad Saúde Pública. 2011 Apr; 27 (4): 623-38.
28. Laurenti R, Jorge MHP de M, Gotlieb SLD. A mortalidade materna nas capitais brasileiras: algumas características e estimativa de um fator de ajuste. Rev Bras Epidemiol. 2004 Dec; 7 (4): 449-60.
Authors’ contributionFerreira RCG, Guedes SC, Moreira RS: conceptualization and design of the study, data collection and analysis, interpretation of results, writing and review of the manuscript. All authors approve the final version of the article and declare no conflicts of interest.
Received on April 20, 2023
Final version presented on September 20, 2024
Approved on September 21, 2024
Associated Editor: Melânia Amorim
 ; Sarah Cavalcanti Guedes 2
; Sarah Cavalcanti Guedes 2 ; Rafael da Silveira Moreira 3
; Rafael da Silveira Moreira 3