ABSTRACT
OBJECTIVES: to evaluate the prevalence and associated factors with acquired syphilis in pregnant women attended at the primary health care in Montes Claros-MG.
METHODS: a cross-sectional study carried out with pregnant women enrolled in the Estratégia Saúde da Família (Family Health Strategy) teams in Montes Claros, Minas Gerais, Brazil (2018-2019). Sociodemographic, behavioral and obstetric factors were collected through a questionnaire applied by interview. The result of the Venereal Disease Research Laboratory (VDRL) examination was evaluated. Binary logistic regression analysis was used to determine associated factors with syphilis in pregnancy.
RESULTS: the prevalence of syphilis found was 1.7% (CI95%= 1.44-1.96). Pregnant women who graduated from high school had 75% (OR = 0.25; CI95%= 0.08-0.81) less chance of having syphilis, when compared to pregnant women with elementary school. Pregnant women who used illicit drugs during pregnancy (OR = 3.47; CI95%= 1.02-11.82) and consumed alcoholic beverages during pregnancy (OR = 16.35; CI95%= 3. 81-70.20) were more likely to have the disease.
CONCLUSION: schooling, consumption of alcohol and illicit drugs are associated with the diagnosis of syphilis in pregnant women. Therefore, educational programs and interventions are needed to address issues related to prevention, diagnosis, treatment and their risk factors, especially social determinants, and women's reproductive health issues.
Keywords:
Gestational syphilis, Prenatal care, Risk factors, Infectious diseases
RESUMO
OBJETIVOS: avaliar a prevalência e fatores associados à sífilis adquirida em gestantes atendidas na atenção primária à saúde de Montes Claros-MG.
MÉTODOS: trata-se de um estudo transversal realizado com gestantes cadastradas nas equipes da Estratégia Saúde da Família de Montes Claros, Minas Gerais, Brasil (2018-2019). Fatores sociodemográficos, comportamentais e obstétricos foram coletados por meio de questionário aplicado por entrevista. Foi avaliado o resultado do exame Venereal Disease Research Laboratory (VDRL). Uma análise de regressão logística binária foi usada para determinar os fatores associados à sífilis na gestação.
RESULTADOS: a prevalência de sífilis encontrada foi de 1,7% (IC95%= 1,44-1,96). Gestantes com ensino médio tiveram 75% (OR = 0,25; IC95% = 0,08-0,81) menos chance de ter sífilis, quando comparado a gestantes com ensino fundamental. Gestantes que fizeram uso de drogas ilícitas antes da gestação (OR = 3,47; IC95%= 1,02-11,82), e consumiram bebidas alcoólicas durante a gestação (OR = 16,35; IC95%= 3,81-70,20) apresentaram maior chance de ter a doença.
CONCLUSÃO: a escolaridade, o consumo de álcool e drogas ilícitas estão associados ao diagnóstico de sífilis em gestantes. Portanto, são necessários programas e intervenções educativas para abordar questões relacionadas à prevenção, diagnóstico, tratamento e os seus fatores de risco, sobretudo, os determinantes sociais e as questões de saúde reprodutiva das mulheres.
Palavras-chave:
Sífilis gestacional, Cuidado pré-natal, Fatores de risco, Doenças infecciosas
IntroductionGlobally, 36 million people are infected with syphilis and two million of these are pregnant women.
1 Syphilis is a sexually transmitted infection (STI), whose etiologic agent is the bacterium Treponema pallidum, first identified in 1905 by German scientists, and after a year, the first test for its diagnosis was developed.
2 Despite, widely available testing and treatment methods, gestational syphilis is still considered one of the main public health problems worldwide.
3Disease transmission occurs mainly through unprotected sexual intercourse (acquired syphilis), and can also be transmitted from mother to child during pregnancy, via the transplacental route, or during passage through the birth canal (congenital syphilis).
2,4,5Gestational syphilis can have serious implications, such as miscarriage, stillbirth, neonatal death, premature births, low birth weight babies and various early and late clinical complications in live births.
1,6 It can also compromise women’s quality of life, mental health and reproductive health.
7Brazil is experiencing an increase in syphilis cases, declared as a public health emergency in 2016, mainly affecting pregnant women and newborns. The detection rate of syphilis cases in pregnant women increased from 13.4 in 2016 to 21.6 in 2020, where 61,441 syphilis cases in pregnant women and 22,065 congenital syphilis cases were reported.
8The recommendations for controlling the disease reinforce interventions aimed at preventing and diagnosing syphilis. The factors that contribute to women acquiring syphilis are related to various socioeconomic, behavioral and healthcare factors, such as: younger age, non-white race/color, low schooling, living in rural areas, drug, alcohol and smoking use, a history of STIs, abortions, multiple sexual partners, late and low-quality prenatal care, among others.
9-13Brazil is a reference in the implementation of actions to tackle syphilis based on the adoption of effective public policies to reduce cases of the infection, in line with the
Objetivos de Desenvolvimento Sustentável (Sustainable Development Goals) in relation to the 2030 Agenda.
14 And even with 95% coverage of prenatal care and screening for syphilis in pregnant women, there is still a high incidence of this disease and it impacts on public health.
15Knowledge and understanding of the syphilis epidemiology and its risk factors are important to enhance education and prevent measures for the most vulnerable groups, the evaluation of actions to reduce vertical transmission of syphilis, and the organization of the health system and services.
16In this context, the aim of this study was to assess the prevalence and associated factors with acquired syphilis in pregnant women attending primary health care (PHC) in Montes Claros-MG, Brazil.
MethodsThis is an epidemiological, cross-sectional, analytical study conducted with data from a larger study entitled ALGE - Evaluation of the Health Conditions of Pregnant Women in Montes Claros - MG: a longitudinal study conducted with pregnant women registered with the
Estratégia Saúde da Família (ESF) (Family Health Strategy) teams in the urban area of the city of Montes Claros, in the North of Minas Gerais, Brazil.
The total population of the ALGE study was 1,279 pregnant women registered with the ESF teams in the urban area of the city of Montes Claros in 2018. The sample size was established in order to estimate population parameters with a prevalence of 50% (to maximize the sample size and because the project included several events), a 95% confidence interval (CI95%) and a precision level of 2.0%. Correction was made for a finite population (N=1,661 pregnant women) and an addition of 20% was also established to compensate for possible non-response and losses.The calculations showed that at least 1,180 pregnant women needed to take part. However, only 823 pregnant women (64.3%) provided Venereal Disease Research Laboratory (VDRL) test results, thus forming the sample for this study.
To select the sample, the ESF centers in the city were taken into account, which totaled 15 at the time of this study. The number of pregnant women sampled at each center was proportional to their representativeness in relation to the total population of registered pregnant women. We included pregnant women who were registered at a ESF of the PHC at any gestational age and excluded women who were pregnant with twins and those with cognitive impairment, according to information from the family member and/or the ESF team.
As for the data collection process, the coordination managers of the PHC and the ESF in the city were initially contacted to raise awareness and explain the purpose of the research. Once they had agreed, the ESF professionals responsible for prenatal care provided a list of pregnant women in their area of coverage containing their names, telephone numbers and addresses. Once they had these lists, a team of interviewers made initially telephone contact with the women, inviting them to come forward and raise awareness of the study, and then scheduled and carried out the data collection. Data collection took place between October 2018 and November 2019, at the ESF health units or at the participant’s home, depending on their availability.
A multi-professional team made up of health professionals and undergraduate students was responsible for the previously trained interviews, which took place face-to-face.
This study analyzed: (1) sociodemographic characteristics (age group, skin color, marital status, schooling, religious, occupation, family income, number of rooms and number of people in the house) (2) obstetric variables (pregnancy planning, number of pregnancies, previous abortions, prenatal care and number of appointments) (3) behavioral variables (use of licit and illicit drugs) and the outcome variable “diagnosis of syphilis during pregnancy” (VDRL test).
In order to evaluate the laboratorial tests, the research instrument used was a questionnaire containing questions with objective answers about prenatal issues relating to laboratorial tests. Initially, the intention was to identify whether the pregnant woman had access to request for laboratorial tests and which tests were carried out during prenatal care in each trimester. As for serologies, the pregnant woman was asked if she had been tested for Syphilis, Hepatitis B, HIV and Toxoplasmosis. In the case of the VDRL test, the titre of the test was assessed (from titres of 1:1 it is considered reactive) or qualitatively (reactive or non-reactive), as recorded on the pregnant woman’s card.
Simple and relative frequencies were used to describe the characteristics of the study population. The magnitude of the association between the dependent variable “diagnosis of syphilis during pregnancy” and the other variables investigated was estimated by means of the odds ratio (OR), using the binary logistic regression model. Initially, bivariate analyses were carried out (Pearson’s chi-squared test) and the variables that showed a descriptive level (
p-value of up to 0.25) were selected for the multiple model, with a significance level of 0.05.
It should be noted that the assumption of multicollinearity was checked and there was no autocorrelation between the variables. The quality of the final model was analyzed using the Hosmer and Lemeshow test.
All the analyses were carried out using the statistical program Statistical Package for the Social Science (SPSS), Windows version 20.0® (SPSS for Windows, Chicago, USA).
This research project was approved by the Research Ethics Committee of the
Universidade Estadual de Montes Claros, with substantiated opinion number 2.483.623/2018, CAAE 80957817.
ResultsA total of 823 women took part in this study, most were aged between 21 and 30 (48.9%), self-declared as non-white (88.6%), with more than eight years of schooling (65.0%) and considered moderately religious (52.2%). With regard to marital status, 637 (79.5%) women had partners, 62.9% lived in homes with five or fewer rooms, the most (59.3%) lived with up to three p0eople in the home, and 42.1% had a family income of up to 1,000 reais per month and 35.2% between 1,001 and 2,000 reais.According to occupational category, more than half of the participants were housewives (53.9%), about 35.5% received salary and
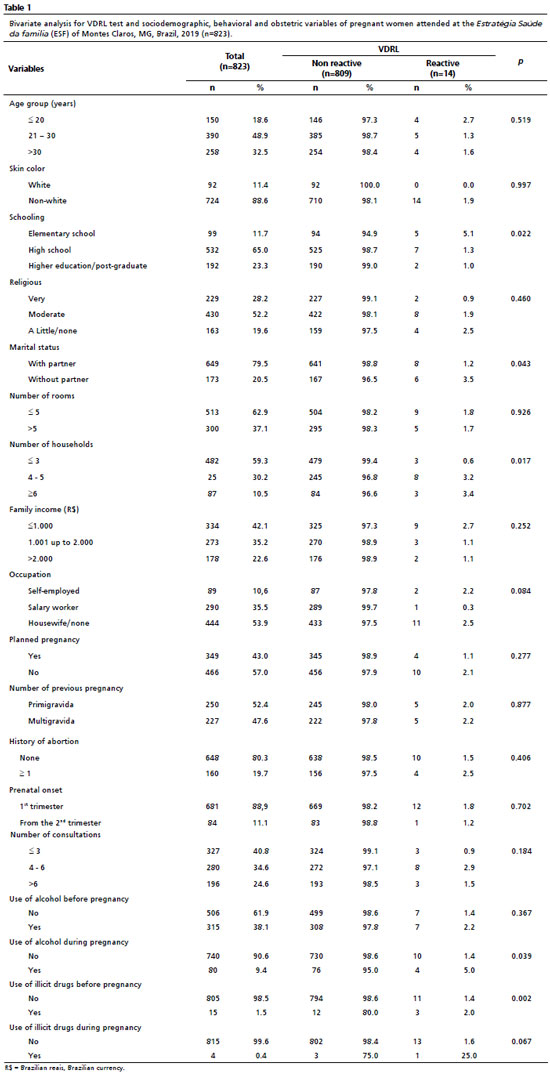
With regard to obstetric and behavioral variables, more than half (57.0%) of the participants had not planned the pregnancy, 52.4% of the women were primigravidas, 19.7% reported had an abortion, 88.9% started prenatal care in the first trimester of pregnancy and, at the time of data collection, 40.8% of the participants had had up to three prenatal consultations and 24.6% more than six. Before the pregnancy, 38.1% of the women consumed alcohol and 1.5% other illicit drugs. During pregnancy, these percentages fell to 9.4% and 0.4%, respectively (Table 1).
The prevalence of syphilis among the participants was 1.7% (VDRL reactive result). In the bivariate analysis, the variables that were associated (
p<0.25) with the occurrence of syphilis during pregnancy were: schooling (
p=0.022), marital status (
p=0.043), number of people in the household (
p=0.017), household income (
p=0.252), occupation (
p=0.084), number of prenatal consultations (
p=0.184), alcohol consumption during pregnancy (
p=0.039), use of illicit drugs before pregnancy (
p=0.002) and during pregnancy (
p=0.067) (Table 1).
Table 2 shows the results of the multivariate analysis. Pregnant women graduated from high school were 75% (OR=0.25; CI95%=0.08-0.81) less likely to have syphilis compared to pregnant women with an elemenatary schooling. The use of alcoholic beverages during pregnancy (OR=3.47; CI95%=1.02-11.82) and the use of illicit drugs before pregnancy (OR=16.35; CI95%=3.81-70.20) were the associated factors with a higher risk of syphilis.
DiscussionThe findings of this study show that 1.7% of pregnant women undergoing prenatal care at the ESF in Montes Claros, in the North of Minas Gerais, were infected with syphilis. This prevalence is lower than that observed in studies carried out in the Zona da Mata Mineira and in the South and Midwest regions of Brazil.
17,13,10 In the national context, the prevalence of gestational syphilis has increased significantly over the years. According to data from the Ministry of Health, syphilis detection rate was 5.7% in 2012, reaching 27.1% in 2021.
18 This significant increase can be attributed to the increase in prenatal care coverage and syphilis screening across the country.
It is interesting to note that, despite differences in accessibility to health services, risk behaviors and awareness of syphilis infection, the prevalence found in this study is similar to those reported in international studies were carried out in India, Ethiopia and South Africa.
19,3,11In relation to the pregnant women’s sociodemographic profile, the findings are similar to other studies in which the majority of women were non-white, had completed high school, had a partner and were housewives.
10,13,17,20 With regard to obstetric variables, Guedes
et al.17 found similar data regarding to a history of miscarriage, starting prenatal care in the first trimester of pregnancy and having six or more appointments.
When evaluating the associated factors with a diagnosis of syphilis, this study found that a higher level of schooling reduced the chances of the pregnant woman having the disease by 75%. Biswas
et al.19 found that the prevalence of syphilis was higher among illiterate pregnant women, with a gradual reduction in the chance of having syphilis as schooling improved. Low schooling has been identified as a risk factor for syphilis in several studies,
13,16,21,22 suggesting that this group is more exposed to infection due to less access to information and a limited understanding of the importance of health care, and should therefore receive greater attention from syphilis control programs during pregnancy.
16,23,24A study carried out by Attanasio
et al.25 shows that even pregnant women diagnosed with syphilis did not have sufficient knowledge about what the disease is and how to prevent it, with little knowledge being acquired only after confirmation of syphilis. This is due to difficulties associated with the social context in which women live, such as a low level of schooling and lack of prior knowledge about the disease, as well as a possible failure of the health system in public policies aimed at syphilis prevention and health education for the population.
25,26 In this context, it should be noted that PHC plays a fundamental role in tackling vertical transmission of syphilis in pregnant women, as it is the main gateway to health services and can help change the epidemiological picture of gestational syphilis.
This study showed that participants who consumed alcohol during pregnancy were 3.47 times more likely to be infected with syphilis. Corroborating this, a study by Enbiale
et al.12 showed that pregnant women who consumed alcohol were three times more likely to be seropositive for syphilis than women who did not consume alcohol.
Furthermore, this study found that the chance of having syphilis was 16.35 times higher among pregnant women who had used illicit drugs before pregnancy. Previous studies have also found that the use of illicit drugs resulted in a significant increase in the risk of developing syphilis in pregnant women. For example, while a study carried out in Mato Grosso do Sul, a State in the Midwest region of Brazil, found a 13-fold increase in risk, other studies in Brazil and Ethiopia showed that illicit drug use increased the chance of women having gestational syphilis by more than three times.
10,21,20Exposure to syphilis via sexual route is the most common, like any other STI.
27 Alcohol and drug use increases the likelihood of a person having multiple sexual partners, not using condoms, reducing the perception of the risk of contamination and increasing the risk of unwanted pregnancies.
10 In addition, according to Lendado et al.
20 pregnant women with a history of drug use tend to be reluctant to attend prenatal care, get tested and follow treatment for syphilis.
Investigating the association between low schooling and the consume of alcohol and illicit drugs with the prevalence of syphilis in pregnant women found in this study provides useful information for public health. It reinforces that the epidemiological dynamics of syphilis in society encompass a multiplicity of factors that condition situations of vulnerability imposed by social and economic factors, such as access to education, family income and place of residence, reflecting access to health services.
28This study had some limitations in its development, such as the use of secondary data (prenatal card), subject to the quality of the records.The results achieved do not represent the serological situation of the population of pregnant women in the city of Montes Claros, as the study only included those who had prenatal care at the Montes Claros PHC, which could underestimate the real incidence of congenital syphilis in the city.
Schooling and the consumption of alcohol and illicit drugs are associated with the diagnosis of syphilis in pregnant women. Therefore, educational programs and interventions are needed to address issues related to the prevention, diagnosis and treatment on syphilis and its risk factors, especially social determinants and women’s reproductive health issues.
References1. World Health Organization (WHO). Report on global sexually transmitted infection surveillance. Geneva: WHO; 2018. [access in 2023 Jan 10]. Available from:
https://www.who.int/publications/i/item/97892415656912. Kojima N, Klausner JD. An Update on the Global Epidemiology of Syphilis. Curr Epidemiol Rep. 2018; 5 (1): 24-38.
3. Genetu K, Abere K, Tachbele E. Magnitudes and Correlates of Human Immunodeficiency Virus, Hepatitis B Virus, and Syphilis among Pregnant Mothers Attending Antenatal Care in Addis Ababa, Ethiopia. Infect Dis Obstet Gynecol. 2022; 2022 (1): 6156613.
4. Yitbarek GY, Ayele BA. Prevalence of Syphilis among Pregnant Women Attending Antenatal Care Clinic, Sede Muja District, South Gondar, Northwest Ethiopia. J Pregnancy. 2019; 2019: 1584527.
5. Valentim RAM, Caldeira-Silva GJP, Silva RD, Albuquerque GA, Andrade IGM, Sales-Moioli AIL,
et al. Stochastic Petri net model describing the relationship between reported maternal and congenital syphilis cases in Brazil. BMC Med Inform Decis Mak. 2022; 22 (1): 40.
6. Medeiros JAR, Yamamura M, Silva ZP, Domingues CSB, Waldman EA, Chiaravalloti-Neto F. Spatiotemporal dynamics of syphilis in pregnant women and congenital syphilis in the state of São Paulo, Brazil. Sci Rep. 2022; 12 (1): 585.
7. Tavares CSS, Oliveira SJGS, Gois-Santos VT, Vaez AC, Menezes MO, Santos Jr HP,
et al. Quality of life, depressive symptoms, anxiety, and sexual function in mothers of neonates with congenital syphilis in Northeast Brazil: A cohort study. Lancet Reg Health Am. 2022; 7: 100127.
8. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Vigilância, Prevenção e Controle das IST, do HIV/Aids e das Hepatites Virais – DIAVH/SVS/MS. Boletim Epidemiológico – Sífilis, 2021. Brasília (DF): Ministério da Saúde; 2021. [access in 2023 Jan 10]. Available from:
https://www.gov.br/aids/pt-br/central-de-conteudo/boletins-epidemiologicos/2021/sifilis/boletim_sifilis_2021_internet.pdf/view9. Domingues RMSM, Leal MDC, Pereira APE, Ayres B, Sánchez AR, Larouzé B. Prevalence of syphilis and HIV infection during pregnancy in incarcerated women and the incidence of congenital syphilis in births in prison in Brazil. Cad Saúde Pública. 2017; 33 (11): e00183616.
10. Benedetti KCSV, Ribeiro ADDC, Queiroz JHFS, Melo ABD, Batista RB, Delgado FM,
et al. High Prevalence of Syphilis and Inadequate Prenatal Care in Brazilian Pregnant Women: A Cross-Sectional Study. Am J Trop Med Hyg. 2019; 101 (4): 761-6.
11. Hoque M, Hoque ME, Van Hal G, Buckus S. Prevalence, incidence and seroconversion of HIV and Syphilis infections among pregnant women of South Africa. S Afr J Infect Dis. 2021; 36 (1): 296.
12. Enbiale M, Getie A, Haile F, Tekabe B, Misekir D. Magnitude of syphilis sero-status and associated factors among pregnant women attending antenatal care in Jinka town public health facilities, Southern Ethiopia, 2020. PLoS One. 2021; 16 (9): e0257290.
13. Yeganeh N, Kreitchmann R, Leng M, Nielsen-Saines K, Gorbach PM, Klausner J. High Prevalence of Sexually Transmitted Infections in Pregnant Women Living in Southern Brazil. Sex Transm Dis. 2021; 48 (2): 128-33.
14. Almeida MCD, Cordeiro AMR, Cunha-Oliveira A, Barros DMS, Santos DGSM, Lima TS,
et al. Syphilis response policies and their assessments: A scoping review. Front Public Health. 2022; 10: 1002245.
15. Figueiredo DCMM, Figueiredo AM, Souza TKB, Tavares G, Vianna RPT. Relação entre oferta de diagnóstico e tratamento da sífilis na atenção básica sobre a incidência de sífilis gestacional e congênita. Cad Saúde Pública. 2020; 36(3): e00074519.
16. Cavalcante PAdM, Pereira RBL, Castro JGD. Sífilis gestacional e congênita em Palmas, Tocantins, 2007-2014. Epidemiol Serv Saúde. 2017; 26 (2): 255-64.
17. Guedes ALL, Guimarães DCDS, Sarkis DJ, Gabriel TT, Delgado CS, Campos AAL,
et al. Factors associated with women diagnosed with syphilis who received prenatal care in a primary healthcare unit. Einstein (São Paulo). 2023 Mar; 21: eAO0046.
18. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Departamento de Doenças Crônicas e Infecções Sexualmente Transmissíveis. Indicadores de Sífilis nos Municípios Brasileiros. 2022. [access in 2023 Jan 10]. Available from:
http://indicadoressifilis.aids.gov.br/19. Biswas S, Ghosh P, Debnath F, Chakraborty D, Saha MK, Dutta S. Prevalence of syphilis infection and associated sociodemographic factors among antenatal-care attendees in Meghalaya, India: Revisiting HIV Sentinel Surveillance data. Int J STD AIDS. 2022; 33 (2): 173-9.
20. Lendado TA, Tekle T, Dawit D, Daga WB, Diro CW, Arba MA, Tekle T. Determinants of syphilis infection among pregnant women attending antenatal care in hospitals of Wolaita zone, Southern Ethiopia, 2020. PLoS One. 2022 Jun 3 17 (6): e0269473.
21. Macêdo VC, Lira PIC, Frias PG, Romaguera LMD, Caires SFF, Ximenes RAA. Risk factors for syphilis in women: case-control study. Rev Saude Publica. 2017 Aug 17; 51: 78.
22. Padovani C, Oliveira RR, Pelloso SM. Syphilis in during pregnancy: association of maternal and perinatal characteristics in a region of southern Brazil. Rev Lat Am Enferm. 2018 Aug 9; 26: e3019.
23. Domingues RM, Szwarcwald CL, Souza Junior PR, Leal Mdo C. Prevalence of syphilis in pregnancy and prenatal syphilis testing in Brazil: birth in Brazil study. Rev Saúde Pública. 2014 Oct; 48 (5): 766-74.
24. Nonato SMA, Melo ANPS, Guimarães MDCSC. Sífilis na gestação e fatores associados à sífilis congênita em Belo Horizonte-MG, 2010-2013. Serv Saúde. 2015; 24 (4): 681-94.
25. Attanasio JCO, Andrade MEO, Tanure SST, Schacht V, Oliveira YE, Bello CMM,
et al. Avaliação do conhecimento de gestantes e puérperas frente ao cenário da sífilis gestacional em município de Minas Gerais. Rev Med Minas Gerais. 2021; 31 (Supl. 5): S67-S73.
26. Lima LE, Xavier AMH, Almada CB. Conhecimento das gestantes com sífilis sobre a doença e perfil sociodemográfico em uma UBS e Hospital Maternidade da zona norte de São Paulo. J Health Sci Inst. 2019; 37 (3): 218-23.
27. Meneses MO, Vieira BDG, Queiroz ABA, Alves VH, Rodrigues DP, Silva JCS. O perfil do comportamento sexual de risco de mulheres soropositivas para sífilis. Rev Enferm UFPE online. 2017; 11 (4): 1584-94.
28. Mélo KC, Santos AGGD, Brito AB, Aquino SHS, Alencar ÉTDS, Duarte EMDS,
et al. Syphilis among pregnant women in Northeast Brazil from 2008 to 2015: a trend analysis according to sociodemographic and clinical characteristics. Rev Soc Bras Med Trop. 2020; 53: e20190199.
Authors’ contributionEsméria Neta M, Oliveira e Silva C, Silva Jr RF, Eleutério TP, Holzmann APF, Ruas EFG and Marques LO: conception, structuring, data analysis and interpretation, critical review of the manuscript. All the authors have approved the final version of the article and declared no conflicts of interest.
Received on November 6, 2023
Final version presented on August 24, 2024
Approved on August 29, 2024
Associated Editor: Melânia Amorim
 ; Carla Silvana de Oliveira e Silva 2
; Carla Silvana de Oliveira e Silva 2 ; Rene Ferreira da Silva Junior 3
; Rene Ferreira da Silva Junior 3 ; Tatiane Palmeira Eleutério 4
; Tatiane Palmeira Eleutério 4 ; Ana Paula Ferreira Holzmann 5
; Ana Paula Ferreira Holzmann 5 ; Edna de Freitas Gomes Ruas 6
; Edna de Freitas Gomes Ruas 6 ; Luciano Oliveira Marques 7
; Luciano Oliveira Marques 7