ABSTRACT
OBJECTIVES: to analyze the incidence of prematurity in users of a health insurance plan; to analyze the associated risk factors.
METHODS: a retrospective study was conducted in five maternity hospitals with puerperal women who were users of health insurance plans by telephone interviews guided by a semi-structured questionnaire. The variables studied were related to sociodemographic, clinical and outcome conditions. Univariate and multivariate analysis with Backward logistic regression was performed.
RESULTS: 1,193 participants were evaluated and 116 premature births were identified. It was found that preterm birth (p<0.001; OR=4.596; CI95%=2.544-8.305), oligohydramnios (p=0.019; OR=2.697; CI95% =1.140-6.380), diabetes mellitus prior to pregnancy (p<0.001; OR=4.897; CI95%=2.147-11.169), twin pregnancy (p<0.001; OR=7.115; CI95%=3.578-14.148), autoimmune disease (p<0.001; OR=3.799; CI95%=1.987-7.260), stress during pregnancy (p=0.026; OR=1.568; CI95%=1.053-2.335), urinary infection (p=0.008; OR=1.825; CI95%=1.161-2.867), placenta previa (p=0.001; OR=3.180; CI95%=1.517-6.667), pre-eclampsia (p<0.001; OR=4.833; CI95%=2.860-8.169), gestational bleeding (p=0.001; OR=2.185; CI95%=1.340-3.564), interval between pregnancies less than six months (p=0.001; OR=3.502; CI95%=1.594-7.698), pregnancy resulting from in vitro fertilization (p<0.001; OR=2.874; CI95%=1.466-5.637) were statistically relevant as risk factors for prematurity.
CONCLUSION: knowledge of these factors may be important in developing strategies to improve the assistance offered to pregnant women by the health insurance providers.
Keywords:
Premature birth, Pregnancy high-risk, Risk factors, Insurance health
RESUMO
OBJETIVOS: analisar a incidência de prematuridade em usuárias de uma operadora de planos de saúde; analisar os fatores de risco associados.
MÉTODOS: estudo retrospectivo, realizado em cinco maternidades com puérperas usuárias de planos de saúde por meio de entrevistas telefônicas guiadas por questionário semiestruturado. As variáveis estudadas foram relativas às condições sociodemográficas, clínicas e de desfecho. Realizou-se análise uni e multivariada com regressão logística Backward.
RESULTADOS: foram avaliadas 1193 participantes e identificados 116 nascimentos prematuros. Verificou-se que prematuro prévio (p<0,001; OR=4,596; IC95%=2,544-8,305), oligodrâmnio (p=0,019; OR=2,697; IC95%=1,140-6,380), diabetes mellitus anterior a gestação (p<0,001; OR=4,897; IC95%=2,147-11,169), gestação de gemelares (p<0,001; OR=7,115; IC95%=3,578-14,148), doença autoimune (p<0,001; OR=3,799; C95%=1,987-7,260), estresse durante a gestação (p=0,026; OR=1,568; IC95%=1,053-2,335), infecção urinária (p=0,008; OR=1,825; IC95%=1,161-2,867), placenta prévia (p=0,001; OR=3,180; IC95%=1,517-6,667), pré-eclâmpsia (p<0,001; OR=4,833; IC95%=2,860-8,169), sangramento gestacional (p=0,001; OR=2,185; IC95%=1,340-3,564), intervalo entre gestações menor que seis meses (p=0,001; OR=3,502; IC95%=1,594-7,698), gestação proveniente de fertilização in vitro (p<0,001; OR=2,874; IC95%=1,466-5,637) foram estatisticamente relevantes como fatores de risco para prematuridade.
CONCLUSÃO: o conhecimento desses fatores pode ser importante na elaboração de estratégias para melhorar a assistência ofertada às gestantes por operadoras de planos de saúde.
Palavras-chave:
Prematuridade, Gestante de risco, Fatores de risco, Seguro saúde
IntroductionPremature or preterm birth is defined as birth occurring after 20 weeks and before 37 weeks of gestation or 259 days of gestational age.
1 With regard to classification by gestational age, prematurity can be subdivided into: extreme prematurity (<28 weeks); very prematurity (28 to <32 weeks); moderate prematurity (32 to <34 completed weeks) and late prematurity (34 to <37 completed weeks).
2Recent data from the World Health Organization (WHO) show that, globally, the prevalence of premature births ranges from 5% to 18%, and that every year around 15 million babies are born prematurely, which represents 11.1% of live births worldwide.
3 In Brazil, around three million births occur every year, of which 279,000 are preterm births (9.3%).
4Prematurity can be classified as: spontaneous, resulting from spontaneous labor or premature rupture of membranes, or elective, when it is medically indicated due to complications with the fetus or the mother.
5The etiology of preterm birth is multifactorial and often not fully understood. Several risk factors may be involved in this process.
6 Among the situations that increase the occurrence of birth before the adquate moment, the following are: maternal age below 16 or above 35, previous preterm labor, previous abortion,
7,8 asymptomatic bacteriuria or urinary tract infection, unhealthy working conditions,
7 periodontal disease
9 gestational interval of less than six months,
10 oligohydramnios,
11 assisted reproduction,
12 gestational bleeding
8 and post-traumatic stress syndrome.
8,9Comparing to full-term babies, premature newborns are more prone to respiratory problems, difficulties in starting to feed and complications during hospitalization, such as hypothermia, hypoglycemia and hyperbilirubinemia. In addition, there is an increased risk of neonatal mortality and impaired neurological development in the long term.
13 The economic cost of premature birth is also high in terms of the ongoing neonatal intensive care and ongoing health care is required after its occurrence.
9 These costs are high both in the public service and as in the health insurance providers (HIP).
In this sense, it is extremely important to recognize pregnant women with risk factors and try, through adequate prenatal care, to rule out these conditions or minimize their impact during pregnancy, in order to avoid future complications for the newborn.
14 It should be stressed that in Brazil, there is still no systematically collected information, through standardized databases for recording hospital obstetric and neonatal care, with wide coverage, which includes supplementary care, as in developed countries. Therefore, it is important to carry out specific population studies with primary data collection. However, this study aimed to analyze the incidence of prematurity and the associated risk factors among users of a HIP.
MethodsThis is a retrospective observational cohort study. It was carried out in all the maternity hospitals (n=5) served by a HIP in the city of Curitiba-PR, using interviews guided by a semi-structured questionnaire. The study participants were puerperal women who gave birth during the data collection period (September 2021 and July 2022), who were contacted by telephone and agreed to take part in the study. Those who did not want to answer the questionnaire or who could not be contacted within 30 days of giving birth were excluded.
The sample was sequential and by convenience through a single nurse who was masked to the prematurity outcome. The administrative capacity of the HIP did not allow the collection for all the puerperal women.
During one year there were a total of 6,218 deliveries at the HIP and, during the study period, there were 5,181 deliveries. A total of 1,193 puerperal women were randomly included from all the maternity hospitals served by the HIP.
The data was collected using a specific instrument, which contained sociodemographic variables (age, level of schooling), clinical variables (height, weight before pregnancy and at delivery, number of pregnancies, number of previous cesarean sections, number of previous normal deliveries, number of miscarriages and fetal deaths, previous miscarriage, previous premature birth, placenta previa, pre-eclampsia, twin pregnancies, gestation interval of less than six months, in vitro fertilization pregnancies, oligohydramnios, diabetes mellitus prior to pregnancy, gestational diabetes, bleeding during pregnancy, drug use, unhealthy conditions, COVID-19 during pregnancy, periodontal disease, kidney disease, autoimmune disease, sexually transmitted infections, urinary tract infection, procedure on the uterus or cervix during pregnancy, stress during pregnancy, history of heart and lung disease, epilepsy, COVID-19 vaccination, which vaccination and support network), and outcome (premature birth). A new variable was created called number of risk criteria, for which the number of criteria was calculated, counting one point for each criterion presented by the puerperal woman.
All data collection was carried out by a nurse trained by the research team, only by telephone within 30 days of delivery.
The data collection was transferred to the spreadsheets and processed using the Statistical Package for the Social Sciences (SPSS for Windows, version 21.0).
When describing the participants, categorical data was expressed as percentages and continuous variables as means and standard deviations. To assess any differences between the groups, the χ
2 test or Fisher’s exact test were used bilaterally, with
p<0.005 being considered. Univariate and multivariate odds ratios (OR) and 95% confidence intervals (CI) were also calculated. In order to create a predictive model, the variables with
p<0.10 in the univariate analysis were included in a logistic regression with Backward analysis.
The variables included in step one of the logistic regression were: age; age group; height; weight before pregnancy; Body Mass Index (BMI) before delivery; weight before delivery; BMI at delivery; malnutrition; number of previous pregnancies; number of previous normal deliveries; number of previous cesarean sections; number of previous abortions or fetal deaths; age over 35; previous abortion; previous prematurity; drug use; unhealthy conditions; birth complications; Covid-19 in pregnancy; oligohydramnios; gestational diabetes; twins; diabetes mellitus prior to pregnancy; periodontal disease; kidney disease; autoimmune disease; reported stress; placenta previa; pre-eclampsia; gestational bleeding; sexually transmitted infections; pregnancy with a gestational interval of less than six months; uterine procedure during pregnancy; surgery on the cervix; uterine infection; history of heart disease; history of lung disease; epilepsy; previous eclampsia; pregnancy from in vitro fertilization; number of risk criteria; support network; vaccination against Covid-19; which vaccine performed and number of urinary tract infections.
Due to a failure to fill in the questionnaire, the analysis was carried out on the data that was available for each variable, which caused a difference in the total number of pregnant women and newborns in some data, but without compromising the statistical analysis of the work.
The study complied with the National ethics standards for research involving human beings and was approved by the
Universidade Positivo Research Ethics Committee (CAAE: 40447620.7.0000.0093; nº 4.712.895, 14/05/2021).
Results1,193 puerperal women were included. The prematurity rate was 9.7% in the sample studied (n=116). The mothers’ age ranged from 17 to 52, with a mean of 31.91 years (±5.46). There was a predominance of patients who had completed higher education (Table 1).
The maternal risk factors that showed statistical significance in the univariate analysis were previous prematurity (
p<0.001; OR=4.596; CI95%=2.544-8.305), oligohydramnios (
p=0.019; OR=2.697; CI95%=1.140-6.380), diabetes mellitus prior to pregnancy (
p<0.001; OR=4.897; CI95%=2.147-11.169), twin pregnancy (
p<0.001; OR=7.115; CI95%=3.578-14.148), autoimmune disease (
p<0.001; OR=3.799; CI95%=1.987-7.260), stress during pregnancy (
p=0.026; OR=1.568; CI95%=1.053-2.335), urinary infection (
p=0.008; OR=1.825; CI95%=1.161-2.867), placenta previa (
p=0.001; OR=3.180; CI95%=1.517-6.667), pre-eclampsia (
p<0.001; OR=4.833; CI95%=2.860-8.169), gestational bleeding (
p=0.001; OR=2.185; CI95%=1.340-3.564), interval between pregnancies of less than 6 months (
p=0.001; OR=3.502; CI95%=1.594-7.698) and in vitro fertilization pregnancies (
p<0.001; OR=2.874; CI95%=1.466-5.637)(Table 2).
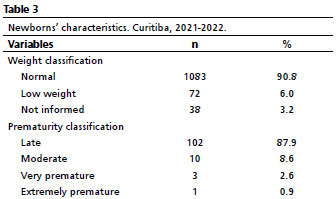
Regarding to the variables related to the newborns, there was a predominance of normal weight (90.8%), and late preterm infants (97.9%) (Table 3).
Table 4 illustrates the variables that were kept in the final logistic regression model and which made it possible to understand the risk factors that are related to the occurrence of prematurity. We highlight the existence of an association between weight before pregnancy (
p=0.005), previous BMI (
p=0.014), weight before delivery (
p=0.005), BMI at delivery (
p=0.007), number of previous cesarean sections (
p=0.015), unhealthy conditions (
p=0.028), pre-eclampsia (
p=0.001) and cervical surgery (
p=0.033) and the occurrence of prematurity.
DiscussionThe incidence of prematurity in this study was 9.7%. It should be noted that in Brazil, the prematurity rate between 2011 and 2021 was 11.1%
15 and has been showing a stable trend. In relation to current options for prevention, these are still limited.
16 In this study, 87.9% of premature babies were classified as late preterm. This condition is considered a risk given the metabolic and neurological immaturity of this group of premature.
16Regard to the age and prematurity variable, many authors agree that women who are 35 or older are more likely to suffer from gestational complications and have greater implications for gestational outcomes and neonatal results.
17 However, this study did not show statistical significance when evaluating this variable in a univariate and multivariate analysis, perhaps because most of the puerperal women included did not fall into the extreme age group.
According to the literature, a previous premature birth increases the risk of having another premature birth by three to four times. The number of recurrence is also associated with a five to six-fold increase in the chance of having a new preterm birth. However, a limitation of this risk marker is that it cannot be applied to nulliparous women.
6 In this study, this risk factor showed statistical significance for the occurrence of prematurity with an OR= 4.596 (CI95%=2.544 - 8.305).
Urinary tract infection (UTI) during pregnancy is common and its prevalence is estimated at 20%.
18 In the sample studied, the rate found was 16.52%. Most UTIs evolve from asymptomatic bacteriuria and can lead to adverse maternal and fetal events.
19 Pregnant women with UTIs can develop preterm labor as a complication, which is related to the increased incidence of prematurity.
20 This risk factor has shown statistical significance for the occurrence of prematurity. It is therefore essential that it is always investigated and treated appropriately.
This study found that oligohydramnios was statistically significant as a risk factor for preterm birth, corroborating another published study.
11 Oligohydramnios can be conceptualized as a marked reduction in the amount of amniotic fluid. This condition has significant consequences for the pregnant woman and her newborn, and the earlier oligohydramnios sets in, the worse the prognosis is.
11Pre-eclampsia was also statistically significant as a risk factor for preterm delivery, corroborating with other authors.
21 Arterial hypertension during pregnancy is defined as systolic pressure ≥140 mmHg or diastolic pressure ≥90 mmHg and can be classified into different syndromes. It is known that hypertensive syndromes in pregnancy can lead to spontaneous labor due to increased uterine contractility. Pre-eclampsia occurs in 2% to 8% of all pregnancies and is the leading cause of maternal death in Brazil, especially when it takes on its severe forms, such as eclampsia and HELLP syndrome.
22The literature mentions that among the many causes that lead to premature birth, special care must be taken with those related to the female genital tract and placental alterations, such as placenta previa.
23 This risk factor showed statistical significance for the occurrence of prematurity in this study.
Corroborating the findings of this study, the short interval between pregnancies (<6 months) should be assessed in every pregnancy, as it is considered a risk factor for prematurity,
10 as well as assisted reproduction,
12 autoimmune disease
25 and Diabetes Mellitus (DM),
23 which are also cited in the literature as risk factors for prematurity.
With regard to assisted reproduction techniques, multiple pregnancy is the most common and most serious iatrogenic complication in this type of procedure. The relation between multiple pregnancies and prematurity is universally recognized, leading to an increase in both maternal and fetal mortality and morbidity.
12Twin pregnancies, stressful situations during pregnancy and gestational bleeding were statistically significant risk factors for preterm birth in this study, corroborating other studies.
8,9,24 Fetal or maternal stress can trigger and release hypothalamic hormones (corticotropin-releasing hormone, oxytocin) and adrenal hormones (cortisol, adrenaline). Bleeding, with the production of thrombin, increases uterine contractility. Uterine hyperdistension is a cause of increased uterine contractility, which occurs in polyhydramnios and twin pregnancies.
1Pregnant women with diabetes have an increased risk of preterm birth due to conditions such as hypertension, infections, increased risk of bleeding, which may be more common in this population, which may lead to the decision to terminate the pregnancy early.
23It should be noted that some studies have shown an association between periodontal disease,
9 previous abortion,
7,8 drug use,
7 Covid-19,
26 kidney disease,
27 sexually transmitted infections
28 and heart disease
8 and premature birth.However, this study did not show statistical significance for the occurrence of prematurity when evaluating these variables.
We reiterate the fact that there were almost 30% of cases of Covid-19 in the sample, but they were not associated with prematurity, perhaps due to the 95.6% vaccination coverage.A retrospective study carried out in China concluded that compared pregnant women without Covid-19, pregnant women with a confirmed diagnosis had an increased risk of premature birth (OR= 3.34; CI95%= 1.60-7.00).
29It should be noted that despite recent technological and scientific developments, with a better understanding of the variables related to prematurity and the definition of new biomarkers associated with preterm birth, the ability of risk scores to predict prematurity still remains weak in most situations, which compromises the integration of a single score for use in clinical practice. The development of new risk scores, the identification of new variables and the development of a large set of reference data from various centers could be a future step towards solving this problem.
30 The regression model presented in this article should be validated in the future within the HIP and in other centers.
This study has some limitations, but these do not restrict its conclusions.The data collection was retrospective and was carried out during the Covid-19 pandemic, which prevented any face-to-face contact; puerperal women attending private maternity hospitals in a single city were included, and it is possible that women giving birth in other maternity hospitals and in the public network have different risks of prematurity; the inability of theHIP to collect data on all deliveries during the study period, which may be due to the lack of contact with many puerperal women, registration errors and, above all, non-response to our telephone calls.
In this study, the risk factors associated with preterm birth were previous prematurity, oligohydramnios, diabetes mellitus prior to pregnancy, twin pregnancy, autoimmune disease, stress during pregnancy, urinary infection, placenta previa, pre-eclampsia, gestational bleeding, interval between pregnancies of less than six months and in vitro fertilization.
Knowing these factors in a given community, as well as comparing them with data from other places, can be important in developing strategies to improve care for the pregnant population.For the HIP, the identification of these factors will enable the implementation of initiatives such as home monitoring and the inclusion of diagnostic laboratory methods in its pregnant women’s program.
References1. Bittar RE. Parto pré-termo. Rev Med (São Paulo). 2018; 97 (2): 195-207.
2. World Health Organization. WHO. Preterm birth. Geneva: WHO; 2015 [access in 2023 Set 8]. Available from:
http://www.who.int/mediacentre/factsheets/fs363/en/3. Organização Mundial da Saúde (OMS). Nascimento prematuro. Genebra: OMS; 2021. [access in 2024 ago 25]. Available from:
https://www.who.int/news-room/fact-sheets/detail/preterm-birth4. Simões AD, Carvalho BCU, Júnior CAS, Alvim CM, Pinheiro, FES, Ferreira GA,
et al. Perfil epidemiológico dos tipos de parto realizados no Brasil: análise temporal, regional e fatorial. Res Soc Dev. 2022; 11 (7): e0211729678.
5. Souza DML, Silva Maia LC, Zêgo ZDF, Jaeger GP, Maciel WS. Prevalência de prematuridade e fatores associados no estado do Rio Grande do Sul. Braz J Health Rev. 2019; 2 (5): 4052-70.
6. Souza RT, Cecatti JG. A Comprehensive integrative review of the factors associated with spontaneous preterm birth, its prevention and prediction, including metabolomic markers. Rev Bras Ginecol Obstet. 2020; 42: 51-60.
7. Dória MT, Spautz CC. Trabalho de parto prematuro predição e prevenção. Femina. 2011.
8. Pohlmann FC, Kerber NP, Viana J, Carvalho VFD, Costa CC, Souza CS. Premature birth: Approaches presents in national and international scientific production. Enferm Global. 2016;42: 410-23.
9. Jacob J, Lehne M, Mischker A, Klinger N, Zickermann C, Walker J. Cost effects of preterm birth: a comparison of health care costs associated with early preterm, late preterm, and full-term birth in the first 3 years after birth. Eur J Health Econ. 2017; 18 (8): 1041-6.
10. Thomazini IFS, Wysocki AD, Cunha MCB, Silva SR, Ruiz MT. Factores de riesgo relacionados conel Trabajo de Parto Prematuro en adolescentes embarazadas: revisión integradora de la literatura. Enferm Global. 2016; 15 (44): 416-27.
11. Freitas RD, Lucena JD, Ogassawara NL, Mendes TPLC, Barros PB, Pelloso SM,
et al. Repercussões perinatais do Oligoidrâmnio na gestação de alto risco. Saúde Colet (Barueri). 2020; 10 (56): 3112-21.
12. Graner VR, Barros SMOD. Complicações maternas e ocorrências neonatais associadas às gestações múltiplas resultantes de técnicas de reprodução assistida. Rev Esc Enferm USP. 2009; 43: 103-9.
13. Seikku L, Gissler M, Andersson S, Rahkonen P, Stefanovic V, Tikkanen M,
et al. Asphyxia, neurologic morbidity, and perinatal mortality in early-term and postterm birth. Pediatrics. 2016; 137 (6).
14. Araújo STH. Fatores de risco materno-fetais para o nascimento pré-termo em hospital de referência de Minas Gerais. Rev Med Minas Gerais. 2020; 30 (Supl. 4): S41-7.
15. Alberton M, Rosa VM, Iser BPM. Prevalência e tendência temporal da prematuridade no Brasil antes e durante a pandemia de covid-19: análise da série histórica 2011-2021. Epidemiol Serv Saúde. 2023; 32: e2022603.
16. Teles JM, Lourenzi Bonilha AL, Tronco CS. Ações de cuidado na maternidade para prematuros tardios. Ciênc Cuid Saúde. 2018; 18 (4).
17. Maia AAA, Pinto APO, Viana JN, Sousa GA, Mourão GG. Fatores de risco da prematuridade: uma revisão narrativa. Rev Eletr Acervo Saúde. 2022; 15 (2): e9711.
18. Hackenhaar AA, Albernaz Elaine Pinto. Prevalência e fatores associados à internação hospitalar para tratamento da infecção do trato urinário durante a gestação. Rev Bras Ginecol Obstet. 2013; 35: 199-204
19. Fernandes FA, Oliveira CNT, Souza CL, Oliveira MV. Relevância do diagnóstico e tratamento da infecção do trato urinário em gestantes: uma revisão da literatura. C&D-Rev Eletron Fainor. 2015; 8 (1): 54-70.
20. Padovani C, Oliveira RRD, Pelloso SM. Sífilis na gestação: associação das características maternas e perinatais em região do sul do Brasil. Rev Lat Am Enferm 2018; 26.
21. Kahhale S, Francisco RPV, Zugaib M. Pré-eclâmpsia. Rev Med (São Paulo). 2018; 97 (2): 226-34.
22. Ramos J, Sass N, Costa S. Pré-eclâmpsia nos seus diversos aspectos. Federação Brasileira das Associações de Ginecologia e Obstetrícia. Série Orientações e Recomendações. FEBRASGO. 2017; (8).
23. Leal MDC, Esteves-Pereira AP, Nakamura-Pereira M, Torres JA, Theme-Filha M, Domingues R. et al. Prevalence and risk factors related to preterm birth in Brazil. Reprod Health. 2016; 13: 163-74.
24. Michaluk A, Dionne MD, Gazdovich S, Buch D, Ducruet T, Leduc L. Predicting preterm birth in twin pregnancy: was the previous birth preterm? A Canadian experience. J Obstet Gynaecol Can. 2013; 35 (9): 793-801.
25. Conde PG, Farhat LC, Braga AL, Sallum AE, Farhat SC, Silva CA. Are prematurity and environmental factors determinants for developing childhood-onset systemic lupus erythematosus?. Mod Rheumatol. 2018; 28 (1): 156-60.
26. Novoa RH, Quintana W, Llancari P, Urbina-Quispe K, Guevara-Rios E, Ventura W. Maternal clinical characteristics and perinatal outcomes among pregnant women with coronavirus disease 2019. A systematic review. Travel Med Infect Dis. 2021; 39: 101919.
27. Zhang JJ, Ma XX, Hao L, Liu LJ, Lv JC, Zhang H. A systematic review and meta-analysis of outcomes of pregnancy in CKD and CKD outcomes in pregnancy. Clin J Am Soc Nephrol. 2015; 10 (11): 1964.
28. Costa MC, Demarch EB, Azulay DR, Périssé ARS, Dias MFRG, Nery JADC. Doenças sexualmente transmissíveis na gestação: uma síntese de particularidades. An Bras Dermatol. 2010; 85: 767-85.
29. Yang R, Mei H, Zheng T, Fu Q, Zhang Y, Buka S, Zhou A. Pregnant women with COVID-19 and risk of adverse birth outcomes and maternal-fetal vertical transmission: a population-based cohort study in Wuhan, China. BMC Med. 2020; 18 (1): 1-7.
30. Ferreira A, Bernardes J, Gonçalves H. Risk Scoring Systems for Preterm Birth and Their Performance: A Systematic Review. J Clin Med. 2023; 12 (13): 4360.
Authors’ contributionsThe authors also contributed to the revision of the article. Author Lind J wrote the initial version of the manuscript.Author Rocha JLL helped with the statistical analysis.All the authors have approved the final version of the article and declare no conflicts of interest.
Received on December 4, 2023
Final version presented on September 2, 2024
Approved on September 3, 2024
Associated Editor: Melânia Amorim
 ; Marcelo de Paula Loureiro2
; Marcelo de Paula Loureiro2 ; Jaime Luis Lopes Rocha3
; Jaime Luis Lopes Rocha3