ABSTRACT
OBJECTIVES: to evaluate the association of episiotomy with pelvic floor function and the occurrence of urinary and fecal incontinence in primiparous adolescents.
METHODS: a cross-sectional study was conducted with primiparous adolescents aged ten to 19 years, seven and 48 months before data collection. Participants completed a form containing their personal data and the International Consultation on Urinary Incontinence (UI) Short Form, Incontinence Severity Index and the Jorge & Wexner Incontinence Scale.
RESULTS: the mean values were statistically significant for the variables analyzed. Lower mean values were obtained for strength, endurance and number of sustained and rapid contractions in the group exposed to episiotomy, compared to the control group. Episiotomy increased the odds of: UI (OR= 15.2; CI95%= 8.1-28.4), UI-related changes in quality of life (OR= 15.9; CI95%= 8.5-30.0), fecal incontinence (OR= 18.5; CI95%= 6.4-5.7) and constipation (OR= 10.8; CI95%= 4.8-24.2) in primiparous adolescents, compared to the control group.
CONCLUSIONS: episiotomy can negatively influence pelvic floor function and urinary and fecal retention. Professionals working in maternal health care should be aware of and reflect on obstetric practices during childbirth in adolescents.
Keywords:
Adolescent, Parity, Episiotomy, Fecal incontinence, Urinary incontinence
RESUMO
OBJETIVOS: avaliar a associação da episiotomia na função do assoalho pélvico e na ocorrência de incontinência urinária e fecal em adolescentes primíparas.
MÉTODOS: foi realizado um estudo transversal, com adolescentes primíparas de dez a 19 anos, de sete e 48 meses pré coleta de dados. As participantes preencheram um formulário contendo seus dados pessoais e ao Questionário da Consulta Internacional sobre Incontinência Urinária (IU) Short Form, Índice de Gravidade da Incontinência e à Escala de Incontinência de Jorge & Wexner.
RESULTADOS: os valores médios foram estatisticamente significativos para as variáveis analisadas. Valores médios mais baixos foram obtidos para força, resistência e número de contrações sustentadas e rápidas no grupo exposto à episiotomia, comparado ao grupo controle. A episiotomia aumentou as chances de: IU (OR= 15,2; IC95%= 8,1-28,4), alteração na qualidade de vida relacionada à IU (OR= 15,9; IC95%= 8,5-30,0), incontinência fecal (OR= 18,5; IC95%= 6,4 -5,7) e constipação intestinal (OR= 10,8; IC95%= 4,8-24,2) em adolescentes primíparas, comparado ao grupo controle.
CONCLUSÕES: a episiotomia pode influenciar negativamente a função do assoalho pélvico e a contenção urinária e fecal. Os profissionais que atuam na atenção à saúde materna devem estar atentos e refletir sobre as práticas obstétricas no parto de adolescentes.
Palavras-chave:
Adolescente, Paridade, Episiotomia, Incontinência fecal, Incontinência urinária
IntroductionEpisiotomy is the most common elective surgical procedure in obstetrics, despite the fact that current scientific evidence does not support its routine use. It is considered one of the main risk factors for the onset of functional changes in the pelvic floor as well as pelvic floor dysfunctions (PFD).
1 The function of the pelvic floor muscles (PFM) is fundamental in the mechanism of urinary and fecal continence. Its essential components are the following: strength, endurance, tone, and control of contraction and muscle relaxation. Alterations in these components may favor the development of PFD.
2PFDs include urinary incontinence (UI) and fecal incontinence (FI). UI is defined by the International Continence Society (ICS) as the involuntary loss of any amount of urine.
3 FI encompasses the involuntary loss of either fecal material or gases at any point in the lifespan of an individual who has already learned to use the toilet.
4Both conditions are considered frequent in the puerperal cycle, with postpartum prevalence of 6% to 31%
6 for UI and 4% to 26%
5,6,7 for FI, according to the characteristics of the investigated population, the employed definitions, and the period in question. Urinary and fecal losses negatively influence women’s quality of life (QoL), as it affects their professional, sexual and leisure activities, besides causing discomfort, shame and fear of having incontinence episodes in public.
4Due to differences in pelvic diameter and PFM tension, as well as fear of the pain and emotional difficulty involved in childbirth, adolescents are at increased risk of episiotomy compared to adult women.
5After searching in several databases (Medline/PubMed, Lilacs/Bireme, Cinahl/Ebsco, Scopus/Elsevier), we were unable to identify any studies with primiparous adolescents that aimed to address the possible influence of episiotomy on the mechanism of urinary and fecal continence. The objective of this study was to evaluate the influence of episiotomy on pelvic floor function and the onset of UI and FI in primiparous adolescents.
MethodsA cross-sectional study was developed at the Physical Therapy Laboratory for Women’s and Pelvic Floor Health (LAFISMA – Portuguese acronym), associated with the Federal University of Pernambuco (UFPE – Portuguese acronym). The sample used here was taken from the database of the study
‘Factors Associated with Urinary Incontinence in Pregnant Adolescents: A Case-Control Study’.
6 This study included primiparous adolescents, aged ten to 19 years and who had previous vaginal delivery between 7-48 months before data collection. Exclusion criteria were cesarean section, multiparity, neurological or renal disease, urogynecological malformation, current or past pelvic cancer, active urinary tract infection, prior urogynecological surgery, not remembering or having records of the required pregnancy and delivery data and.
The Open-epi 3.01 program was used to estimate the study’s sample size. The calculation considered the higher proportion of adolescent episiotomy found in previous Brazilian studies, equal to 40.8%.
7 Episiotomy rates differ among studies depending on geographic region, type of health care service, and sample characterization. Moreover, it is worth emphasizing that no studies whose samples were formed only by primiparous adolescents who had undergone vaginal delivery could be found. As sample parameters, the significance level was set at 5% and 658 as the population.
7 The sample size obtained was composed of 241 volunteers.
Telephone contact was initially established to identify eligible adolescents and schedule their data collection visits at LAFISMA. During in-person meetings, the adolescents received information about the study and signed a consent form, agreeing to participate in the research voluntarily. Adolescents under 18 also had their legal guardians sign a term authorizing their participation.
Afterwards, volunteers filled a form containing sociodemographic, lifestyle, gynecologic-obstetric, anthropometric and associated morbidity data. The gestational and current Body Mass Index (BMI), both expressed in kg/m
2 and converted into qualitative categories, together with the newborn’s weight and gestational age at birth, were obtained by self-report of the adolescent. Physical exercise was considered as the practice of regular physical activities, with a minimum frequency of twice a week and a total duration of 150 minutes per week. Furthermore, the following questionnaires were applied by the evaluator: International Consultation on Incontinence Questionnaire on Incontinence–Urinary Short Form (ICIQ-UISF);
8 Incontinence Severity Index (ISI);
9 and the Jorge & Wexner Incontinence Scale.
10The ICIQ-UI-SF was used to determine the presence and type of UI, confirmed by analyzing question number 6 of the questionnaire, and to assess dysfunction-related QoL. This is a self-administered instrument that received grade-A recommendation by the ICS with regard to its ability to assess UI patients’ QoL. Possible scores range from 0 to 21 points; the higher the score, the higher the impact of UI on QoL.
3To assess UI severity, the ISI was applied, which consists of two questions regarding the frequency and amount of urinary loss. The instrument’s final score is obtained by multiplying urinary loss frequency and amount. Thus, UI can be classified as slight (1–2), moderate (3–6), severe (8–9), or very severe (12).
11The Jorge and Wexner
12 Incontinence Scale was used to assess the degree of FI in adolescents who reported involuntary loss of feces and/or flatus. The instrument consists of a simple scale composed of five questions whose answers can be: 0 – never, 1 – rarely, 2 – sometimes, 3 – usually, 4 – always. The final score ranges from 0 to 20, and FI can be classified as slight (0–7), moderate (8–13), or severe (14–20).
12Constipation was assessed based on the Rome IV criteria; type of FI presented, categorized as: flatus incontinence, liquid fecal incontinence, solid fecal incontinence, passive fecal incontinence, and fecal incontinence during intercourse, according to ICS recommendations;
3 irritative urinary symptoms, classified as: urinary frequency (number of spontaneous urinations greater than or equal to 8 while the volunteer is awake), urinary urgency (a difficult-to-control, strong urge to urinate) and nocturia (need to wake up one or more times to urinate while sleeping), according to ICS recommendations.
3Pelvic floor evaluation was carried out by: measurement of the vulvovaginal opening (distance between the large lips in the vulvar region), classified as: fully closed (0 centimeter), discrete opening (0.1 – 0.5 cm) and accentuated opening (over 0.5 cm);
13 palpation of the perineal body and external anal sphincter, assessed by digital pressure and classified as: normal, hypotonia, or hypertonia; assessment of the presence of voluntary pelvic floor muscle contraction and use of accessory muscles, assessed by bidigital palpation; and assessment of perineal muscle function using the PERFECT scheme.
The PERFECT scheme was employed to assess perineal muscle function, including: quantification of muscle strength – determined by the intensity of voluntary contraction of the pelvic floor, in accordance with the Modified Oxford Scale; endurance –meaning how long muscle contractions are maintained and sustained; number of sustained contractions –meaning the number of contractions sustained for at least five seconds; and number of rapid contractions –i.e., the number of contractions lasting one second.
14 The assessment of the vulvovaginal opening, palpation of the perineal body, external anal sphincter and PERFECT were performed by palpation with the volunteer in the gynecological position. The volunteer was asked to contract the pelvic floor muscles as if to “hold in her pee”. The procedures were performed by members of the research group, who had previously received training and instruction.
Statistical analysis was performed using SigmaPlot 12.0 (
Systat Software, Inc.,
Germany) and IBM SPSS Statistics Software v. 25.0 (SPSS, Inc. IBM Company, New York, US). Continuous variables were expressed as mean and standard deviation. Categorical variables were expressed as number of cases and frequency. The odds ratio (OR) for all categorical variables across the groups was calculated, with their respective 95% confidence intervals (CI95%). To compare continuous variables between groups, Student’s independent t-test or the Mann–Whitney
U test were used. To compare categorical variables between groups, we used the chi-square test or Fisher’s exact test. Significance was considered when
p<0.05.
The study was approved by the Research Ethics Committee of the Center for Medical Sciences of the Federal University of Pernambuco (CAAE: 66720517.3.0000.5208; opinion no. 2.081.488; approved on 05/25/2017).
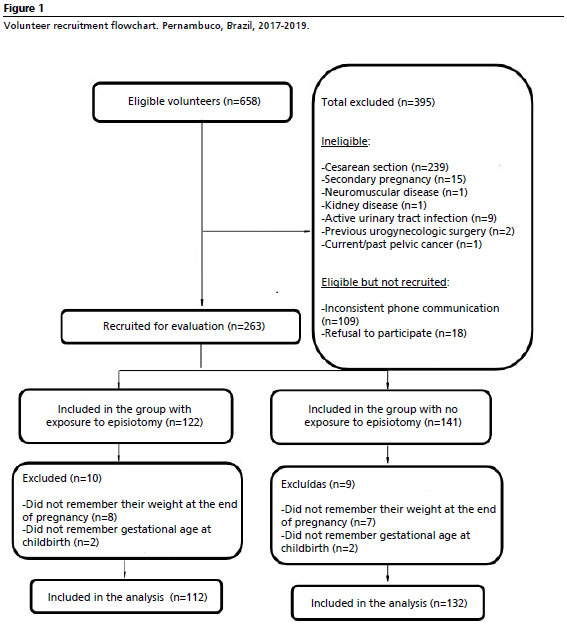
ResultsAmong 658 adolescents, 244 met eligibility criteria and were selected for study participation. The group exposed to episiotomy was composed of 112 adolescents (45.9%), while the non-exposure group consisted of 132 adolescents (54.1%) (Figure 1).
Table 1 presents data on the characterization of the sample of primiparous adolescents according to exposure or non-exposure to episiotomy, considering their sociodemographic variables, lifestyle habits, gynecologic-obstetric and anthropometric data, and associated morbidities.
Variables related to the evaluation of pelvic floor structures are presented in Table 2. Regarding perineal muscle function, mean values of muscle strength, resistance, number of sustained contractions and smaller rapid contractions were recorded in the group exposed to episiotomy as compared to the non-exposure group.
Table 3 presents an analysis of variables related to UI presence, type, severity, impact on dysfunction-related QoL, and irritative urinary symptoms.
Table 4 presents data on FI type and severity, as well as presence of intestinal constipation in the exposure and non-exposure groups.
DiscussionOur results showed an increased chance of functional changes and development of UI and FI after vaginal delivery for primiparous adolescents who underwent episiotomy compared to those who were not subjected to the incision. There are few studies addressing the adolescent population in the context of episiotomy, especially regarding its influence on the development of pelvic floor dysfunction and reduction of perineal muscle function.
Teenage pregnancy is associated with complications such as prematurity, intrauterine growth restriction, small-for-gestational-age newborns, fetal distress, gestational diabetes, preeclampsia, and increased cesarean sections.
15Physical and psychological factors of growth in adolescence, such as slower pelvic development, greater tension in the pelvic floor muscles, and emotional repercussions, increase the prevalence of episiotomy in this population.
16The mean gestational BMI in the third trimester is higher in adolescents undergoing episiotomy, suggesting competition for nutrients between mother and baby, favoring increased BMI and risk of low birth weight. Excessive maternal weight gain increases complications during childbirth, especially in cases of obesity.
17 Although weight gain during pregnancy increases the risk of obstetric interventions, few studies relate high gestational BMI and episiotomy, and none has focused on adolescents.
Adolescents with higher gestational BMI and heavier newborns are at increased risk of pelvic floor dysfunction.
17 Postpartum BMI is also higher in adolescents who have had an episiotomy, with overweight persisting years after delivery. A five-unit increase in BMI increases the risk of urinary incontinence, affecting more than 10% of obese adolescents. The second stage of labor was longer in adolescents who underwent episiotomy.
18The duration of the second stage of labor was greater than 60 minutes in 22% of adolescents who underwent episiotomy, while it was equal to or less than 60 minutes in 99% of those who did not undergo the procedure. In the past, episiotomy was routinely recommended to reduce the expulsive period and prevent perineal damage and birth trauma.
18The lithotomy position was more common among adolescents who underwent episiotomy (97%), while upright positions were more frequent among those who did not (77%). Studies show that vertical positions result in a lower percentage of episiotomy.
2,19Instrumental deliveries and obstetric interventions, such as the use of forceps, vacuum extraction, epidural analgesia and oxytocin, increase the risk of episiotomy. Studies indicate that instrumental deliveries are associated with maternal complications and the performance of episiotomy.
20The average birth weight of newborns of adolescents who underwent episiotomy was higher, with a significant association between episiotomy and neonatal weight above 3,000 grams. Research shows that newborn weight influences perineal integrity, and the risk of severe perineal lacerations increases with neonatal weight above 4,000 grams. Episiotomy is justified in clinical practice due to fetal macrosomia.
21Accentuated vulvovaginal opening was more frequent in the presence of episiotomy, as it results in the weakening of the muscles that make up the pelvic floor (especially the bulbospongiosus and ischiocavernosus muscles).
13 Episiotomy cuts muscles of the pelvic and urogenital diaphragm, in addition to the vaginal mucosa, the navicular fossa epithelium, the skin over the ischioanal fossa, and the fascia and neurovascular bundles, contributing to enlarging the vulvovaginal opening as well as reducing the contraction capacity of the PFM, as observed in our study.
2 A previous research with 4,764 primiparous Chinese women showed that the strength of the pelvic floor muscles was lower among those who underwent episiotomy compared to those who had spontaneous laceration or maintained an intact perineum.
22Hypotonia of the perineal body and external anal sphincter were more common among participants who underwent episiotomy when compared to those who did not undergo the procedure. The perineal body is a fibromuscular mass with a high risk of rupture at delivery, especially in cases of episiotomy and instrumental delivery.
1 In regards to the external anal sphincter, lesions are more frequent as a result of median episiotomy.
2,3We also found lower mean values for all PERFECT scheme variables in the group exposed to episiotomy as compared to the non-exposure group. Episiotomy increases the risk of injury to the levator ani muscle, composed mainly of tonic muscle fibers (70%), which are fundamental for maintaining tone and play a role in the support of the pelvic organs. The remaining 30% correspond to phasic muscle fibers that present intense and reflex muscle contractions in response to increased intra-abdominal pressure, resulting in an efficient urethral closure, which is important for the urinary continence mechanism.
23Episiotomy increased the chance of UI by fifteenfold in primiparous adolescents as compared to those who did not undergo the procedure. We believe that episiotomy contributes to reduced pelvic floor support and reduced ability to maintain urethral pressure, due to connective tissue laceration and nervous stretching.
23The most frequent type of UI in the exposure group was MUI (mixed urinary incontinence), with a higher prevalence of severe UI. Meanwhile, in the non-exposure group, the most frequent type of incontinence was SUI (stress urinary incontinence), with a higher prevalence of moderate UI. SUI is the most prevalent form of postpartum UI, and is closely associated with pelvic floor muscle function. Six months after delivery, women who underwent episiotomy have a more prominent decrease in perineal muscle function versus those with intact perineum or spontaneous first-degree lacerations.
24 In a literature review, Zivkovic
et al.
25 concluded that episiotomy is associated with postpartum UI – especially of the SUI type, but also MUI, since the stress component is included in the latter’s pathophysiological mechanism.
The group exposed to episiotomy had a more than tenfold increase in the chance of urinary frequency, urgency and nocturia, as compared to the non-exposure group. The presence of urinary urgency associated or not with frequency, nocturia, and UUI (urge urinary incontinence) characterizes overactive bladder syndrome (OAB).
3 One is led to question whether the high prevalence of OAB symptoms in adolescents subjected to episiotomy may have been influenced by changes in the voiding cycle due to pudendal nerve injury caused by the incision.
23 However, this hypothesis needs to be further investigated by means of longitudinal studies with complementary examinations.
The mean ICIQ-UI-SF score was higher among adolescents in the group exposed to episiotomy as compared to the non-exposure group, which means that episiotomy negatively influenced adolescents’ QoL perception. The repercussions of UI on women’s lifestyle are numerous, with physical, economic and psychosocial implications, as UI interferes with social, professional, sexual, and family life.
26 The previous study from which our sample was taken reported moderate impact of UI on the QoL of adolescent pregnant women.
27 However, it is important to highlight that negative changes in UI-related perception of QoL may start in pregnancy, persisting and even worsening after pregnancy, according to our results.
We recorded an increased chance of postpartum UI management strategies among adolescents exposed to episiotomy in comparison to adolescents in the non-exposure group. The experience of living with UI leads women to adopt the most diverse behavioral-modification mechanisms, so as to adjust to the inconveniences of urinary loss. Examples are frequent use of perfumes or deodorants to minimize urine odor; dressing with dark clothes; decreased water intake; spontaneous suspension of drugs that stimulate urinary elimination; use of pads or other types of protection to control urinary loss; searching for the toilet immediately after entering public places for the first time, and social avoidance.
28Episiotomy led to a more than eighteen fold increase in the chance of UI in primiparous adolescents, as compared to those who were not subjected to episiotomy. UI can negatively impact women’s lives, causing social isolation, embarrassment, time off work, and psycho-emotional problems.
29 Flatus loss was more common in both groups, with higher prevalence in the group undergoing episiotomy.
There was an increased chance in the use of stool loss protection among adolescents exposed to episiotomy compared to the non-exposure group. The risk of involuntary loss of flatus and/or feces in a social environment brings insecurity, fear and distress to the affected individuals, especially given the discomfort stemming from the odor and noise that accompany the event.
7 It is an embarrassing situation that requires life planning to ensure quick and easy access to the bathroom, as well as the use of intimate protection, besides modifications in the use of medicines and consumption of food.
Constipation prevalence was higher in the group of adolescents who underwent episiotomy compared to the group that was not subjected to the incision. Among factors that may explain the higher prevalence of constipation in women are the damage caused to the pelvic floor muscles and their innervations, which result from childbirth and gynecological surgeries, besides genital prolapses.
12 Regarding childbirth specifically, prolonged labor, episiotomy, cesarean section, and the use of enema and painkillers at birth are factors for an increased risk of constipation.
A limitation of this study was the lack of follow-up of adolescents, so outcomes of interest could be investigated over time. We are currently carrying out a longitudinal study to establish the time for UI cessation in the sample’s adolescents who reported involuntary loss of urine after delivery.
We suspect that an important inclusion would have been the evaluation of psycho-emotional aspects such as anxiety, stress and depression, using validated instruments to analyze their influence on the onset of UI, considering the issue of the immaturity of the neurological centers that control urination. However, since this need became obvious only during the present study’s data analysis phase, we suggest further studies to tackle this objective.
Episiotomy may negatively influence pelvic floor function and the maintenance of urinary and fecal continence in primiparous adolescents. In respect to clinical practice recommendations, this study demonstrated the importance of evaluating the function of the pelvic floor and the presence of dysfunctions – as well as associated symptoms – in this population, together with early referral to physiotherapy treatment and a re-consideration of the current obstetric practices-of-choice for adolescent childbirth, especially when it comes to the routine use of episiotomy.
References1. Jiang H, Qian X, Carroli G, Garner P. Selective versus routine use of episiotomy for vaginal birth. Cochrane Database Syst Rev. 2017 Fev; 2017 (2): CD000081.
2. Handa VL, Blomquist JL, Roem J, Muñoz A, Dietz HP. Pelvic floor disorders after obstetric avulsion of the levator ani muscle. Female Pelvic Med Amp Reconstr Surg]. 2019; 25 (1): 3-7.
3. Haylen BT, Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J,
et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecology J. 2009 Nov; 21 (1): 5-26.
4. Sultan AH, Monga A, Lee J, Emmanuel A, Norton C, Santoro G,
et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female anorectal dysfunction. Int Urogynecology J. 2016; 28 (1): 5-31.
5. Monguilhott JJ, Brüggemann OM, Freitas PF, D’Orsi E. Nascer no Brasil: a presença do acompanhante favorece a aplicação das boas práticas na atenção ao parto na região Sul. Rev Saúde Pública. 2018 Jan; 52: 100.
6. Barbosa L, Kühni D, Vasconcelos D, Sales E, Lima G, Santos M,
et al. Factors associated with urinary incontinence in pregnant adolescents: a case-control study. J Pediatr Adolesc Gynecol. 2018 Ago; 31 (4): 382-7.
7. Enderle CD, Kerber NP, Susin LR, Mendoza-Sassi RA. Avaliação da atenção ao parto por adolescentes em um hospital universitário. Rev Bras Saúde Matern Infant. 2012. Dez; 12 (4): 383-94.
8. Tamanini JTN, Dambros M, D’Ancona CAL, Palma PCR, Rodrigues Netto Jr N. Validação para o português do “International Consultation on Incontinence Questionnaire - Short Form” (ICIQ-SF). Rev Saúde Pública. 2004; 38 (3): 438-44.
9. Pereira VS, Santos JYC, Correia GN, Driusso P. Tradução e validação para a língua portuguesa de um questionário para avaliação da gravidade da incontinência urinária. Rev Bras Ginecol Obstet. 2011; 33 (4): 182-7.
10. Yusuf SAI, Jorge JMN, Habr-Gama A, Kiss DR, Rodrigues, JG. Avaliação da qualidade de vida na incontinência anal: validação do questionário FIQL (Fecal Incontinence Quality of Life). Arq Gastroenterol., 2004; 41(3): 202–8.
11. Sandvik H, Hunskaar S, Seim A, Hermstad R, Vanvik A, Bratt H. Validation of a severity index in female urinary incontinence and its implementation in an epidemiological survey. J Epidemiol Amp Comm Health. Dez 1993; 47 (6): 497-9.
12. Jorge MJ, Wexner SD. Etiology and management of fecal incontinence. Dis Colon Amp Rectum. 1993 Jan; 36 (1): 77-97.
13. Incontinência urinária feminina: assistência fisioterapêutica e multidisciplinar. São Paulo: EDUFRN; 2007. Avaliação Cinético-Funcional; p. 71-122.;
14. Oc O, Nf C, G I. Evaluación funcional del piso pelviano femenino (clasificación funcional). Soc Latino Am Uroginecol Cir Vaginal. 1996; 1: 7-9.
15. Azevedo WF, Diniz MB, Fonseca ESVB, Azevedo LMR, Evangelista CB. Complicações da gravidez na adolescência: revisão sistemática da literatura. Einstein. 2015; 13 (4): 618-26.
16. Seligma NM, Rashid T, Parks AC. Positive psychotherapy. Am Psychol. 2006; 61: 774-88.
17. Racz S, Hantosi E, Marton S, Toth K, Ruzsa D, Halvax L,
et al. Impact of maternal obesity on the fetal electrocardiogram during labor. J Matern Fetal Med. 2016; 29 (22): 3712-6.
18. Amorim MM, Franca Neto A, Leal NV, Melo FO, Maia SB, Alves JN.
et al. Is it possible to never perform episiotomy during vaginal delivery? Obstet Gynecol. 2014; 123 (Supl. 1):38S.
19. Edqvist M. Perineal injuries and birth positions among 2992 women with a low risk pregnancy who opted for a homebirth. BMC Pregnancy Childbirth. 2016 Jul; 16 (1): 196.
20. Steiner N, Weintraub AY, Wiznitzer A, Sergienko R, Sheiner E. Episiotomy: the final cut? Arch Gynecol Obstet. 2012; 286 (6): 1369-73.
21. Sobieray NLEC, Souza BM. Prevalência de episiotomia e complicações perineais quando da sua realização ou não em uma maternidade de baixo risco do complexo HC/UFPR. Arq. Med Fac Cienc Med Santa Casa São Paulo. 2019; 64 (2): 93-9.
22. Zhao Y, Zou L, Xiao M, Tang W, Niu HY, Qiao FY. Effect of different delivery modes on the short-term strength of the pelvic floor muscle in Chinese primipara. BMC Pregnancy Childbirth. 2018 Jul; 18 (1): 275.
23. Moccellin AS, Rett MT, Driusso P. Existe alteração na função dos músculos do assoalho pélvico e abdominais de primigestas no segundo e terceiro trimestre gestacional? Fisioter Pesq. Jun 2016; 23 (2): 136-41.
24. Fleming N, Newton ER, Roberts J. Changes in postpartum perineal muscle function in women with and without episiotomies. J Midwifery Amp Womens Health. 2003; 48 (1): 53-9.
25. Živković K. Effect of delivery and episiotomy on the emergence of urinary incontinence in women: review of literature. Acta Clin Croat. 2016: 615-23.
26. Barentsen JA, Visser E, Hofstetter H, Maris AM, Dekker JH, Bock GH. Severity, not type, is the main predictor of decreased quality of life in elderly women with urinary incontinence: a population-based study as part of a randomized controlled trial in primary care. Health Qual Life Outcomes. 2012; 10 (1): 153.
27. Barbosa L, Cruz T, Carvalho A, Torres E, Porto I, Nascimento K,
et al. Urinary incontinence in pregnant adolescents: a case series. Neurourol Urodyn. 2017 Nov; 37 (4): 1329-35.
28. Hermansen IL, OʼConnell BO, Gaskin CJ. Womenʼs explanations for urinary incontinence, their management strategies, and their quality of life during the postpartum period. J Wound Ostomy Cont Nurs. 2010 Mar; 37 (2): 187-92.
29. Rao SS, Bharucha AE, Chiarioni G, Felt-Bersma R, Knowles C, Malcolm A,
et al. Anorectal disorders. Gastroenterol. 2016 Mai; 150 (6): 1430-42.
Authors’ contributionBabini D, Quirino ML and Delgado A: project development, data collection, data analysis and manuscript writing. Lemos A: project development, data analysis and manuscript writing. All authors approved the final version of the article and declare no conflicts of interest.
Received on February 3, 2024
Final version presented on August 26, 2024
Approved on August 27, 2024
Associated Editor: Melania Amorim
 ; Maria Luci Quirino 2
; Maria Luci Quirino 2 ; Alexandre Delgado 3
; Alexandre Delgado 3 ; Andrea Lemos 4
; Andrea Lemos 4